Introduction: A New Beginning Through Bone Marrow Transplant
Receiving a diagnosis that requires a bone marrow transplant (BMT) can feel overwhelming, filled with medical decisions and emotional challenges. Yet for thousands battling blood cancers and bone marrow disorders, this procedure offers hope and a second chance at life.
This guide explains the bone marrow transplant procedure, recovery, risks, and cost in India. You’ll learn why India has become a leading destination for BMT, combining expert doctors, advanced hospitals, and affordable treatment. Our goal is to provide clear, trustworthy information to help patients, families, and medical tourists navigate this life-changing journey with confidence.

Table of Contents
What is a Bone Marrow Transplant (BMT)?
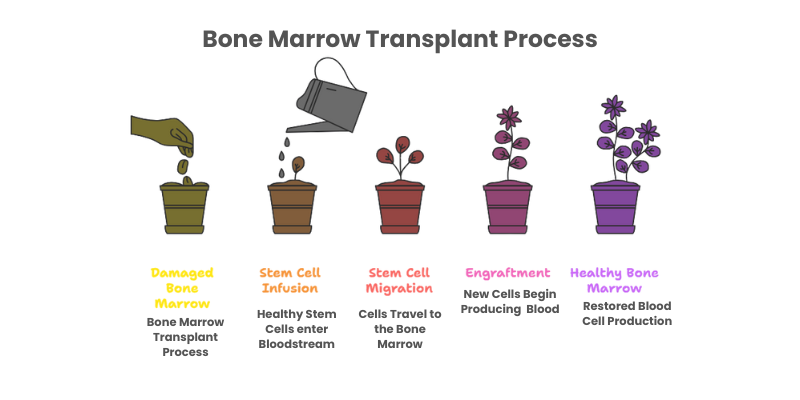
At its core, a bone marrow transplant (BMT) — also called a stem cell transplant — is a procedure that restores the body’s ability to produce healthy blood cells. Bone marrow, the spongy tissue inside the bones, acts as the body’s “blood cell factory,” producing hematopoietic stem cells that develop into red blood cells, white blood cells (to fight infection), and platelets (to control bleeding). According to the Mayo Clinic, when this factory is damaged by disease, infection, or high-dose chemotherapy, a bone marrow transplant procedure replaces it with healthy stem cells, helping the body recover its normal function.
A common misconception is that a bone marrow transplant (BMT) is a major surgery. In reality, the procedure is similar to a blood transfusion. Healthy stem cells are infused into the patient’s bloodstream through a central intravenous catheter. These cells then travel to the bone marrow, where they begin a process called engraftment, producing new and healthy blood cells. As the National Marrow Donor Program (NMDP) explains, this step is not surgery but a critical part of the bone marrow transplant procedure, helping to “reboot” the body’s blood production system.
Types of Bone Marrow Transplants: Finding the Right Match
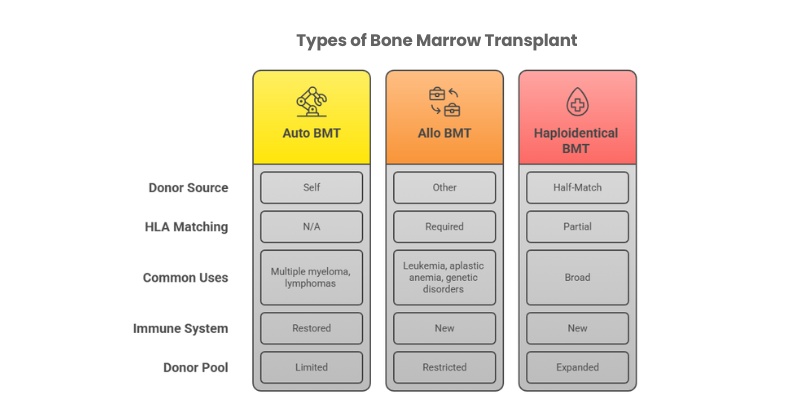
The source of the healthy stem cells determines the type of transplant a patient will receive. The choice depends on the patient’s disease, age, and the availability of a suitable donor. The three primary types are:
- Autologous Bone Marrow Transplant (Auto BMT): The term “auto” means self. In this procedure, the patient serves as their own donor. Before high-dose chemotherapy or radiation, healthy stem cells are collected from the patient’s blood or bone marrow, frozen (cryopreserved), and stored. After treatment destroys the diseased cells, these stem cells are thawed and infused back into the body to restore bone marrow function and rebuild the immune system. According to the American Cancer Society, autologous transplants are commonly used for conditions such as multiple myeloma and certain lymphomas.
- Allogeneic Bone Marrow Transplant (Allo BMT): The term “allo” means other. In this procedure, healthy stem cells come from a donor rather than the patient. To reduce complications, the donor’s Human Leukocyte Antigen (HLA) type must closely match the patient’s. Donors may be siblings, relatives, or volunteers from national and international registries. This type of bone marrow transplant is commonly used to treat conditions such as leukemia, aplastic anemia, and genetic disorders, as it provides not only new stem cells but also a new, healthy immune system from the donor.
- Haploidentical Bone Marrow Transplant (Half-Match BMT): A haploidentical transplant is a type of allogeneic bone marrow transplant that uses a donor who is a 50% HLA match—usually a parent, child, or sibling. Thanks to advanced transplant techniques, doctors can now safely perform these partial-match procedures, greatly expanding the donor pool. This option has been especially valuable for patients from ethnic minorities, who often face challenges in finding a fully matched unrelated donor. Haploidentical transplants have become a game-changer, making bone marrow transplant more accessible to patients worldwide.
Why is a Bone Marrow Transplant Necessary? Conditions Treated
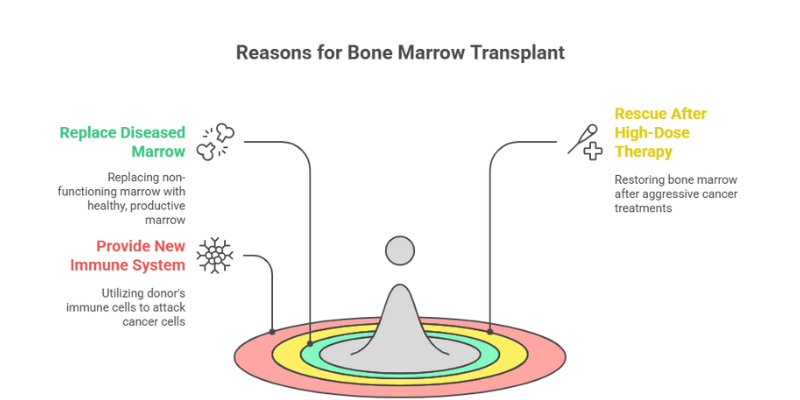
A bone marrow transplant is a powerful, and often curative, therapy that is employed for several critical reasons. The overarching goal is to give the patient a new, healthy hematopoietic system. This is achieved through one of three primary strategies:
- To Replace Diseased Marrow: For conditions where the bone marrow itself is the problem (e.g., aplastic anemia, where it fails to produce blood cells, or myelodysplastic syndromes), a BMT replaces the non-functioning marrow with a healthy, productive one.
- Bone Marrow Transplant After High-Dose Therapy: Some aggressive cancers require very high doses of chemotherapy or radiation that can permanently damage the bone marrow. In these cases, an autologous bone marrow transplant serves as a “rescue” treatment. After the high-dose therapy destroys cancer cells, the patient’s previously collected stem cells are re-infused to restore the bone marrow and rebuild the immune system. This approach is often used in conditions such as lymphoma to improve the chances of long-term remission or cure.
- To Provide a New Immune System (Graft-versus-Tumor Effect): In an allogeneic transplant, the donor’s immune cells can recognize and attack any remaining cancer cells in the patient’s body. This powerful “graft-versus-tumor” or “graft-versus-leukemia” effect is a crucial benefit and one of the main reasons allogeneic transplants are used for blood cancers.
BMT can be a treatment option for over 75 different diseases. The most common conditions treated include:
- Blood Cancers: Acute Myeloid Leukemia (AML), Acute Lymphoblastic Leukemia (ALL), Chronic Myeloid Leukemia (CML), Chronic Lymphocytic Leukemia (CLL), Hodgkin’s Lymphoma, and Non-Hodgkin’s Lymphoma.
- Bone Marrow Failure Syndromes: Severe Aplastic Anemia, Myelodysplastic Syndromes (MDS), and Fanconi Anemia.
- Plasma Cell Disorders: Multiple Myeloma and Primary Amyloidosis.
- Inherited Genetic Disorders: Thalassemia Major and Sickle Cell Disease.
- Other Conditions: Certain immune deficiency disorders and some solid tumors in children, such as neuroblastoma. (Source: BMT InfoNet)
The BMT Procedure: A Step-by-Step Guide
The bone marrow transplant process is not a single event but a carefully orchestrated journey that unfolds over weeks and months. Each phase is critical to success and requires a dedicated, multidisciplinary team of experts. Understanding this timeline can help patients and families prepare for the road ahead.
Stage 1: Pre-Transplant Evaluation & Donor Search
Pre-Transplant Evaluation: Before a bone marrow transplant (BMT), patients undergo a thorough health check to ensure they are strong enough for treatment. This includes blood tests, imaging scans (CT/PET), and assessments of the heart, lungs, liver, and kidneys. According to Jaslok Hospital, this comprehensive evaluation is crucial for determining eligibility. A central venous catheter (central line) is also placed in the chest or neck, which will be used to deliver chemotherapy, medicines, blood products, and later, the new stem cells.
For those having an allogeneic transplant, this phase also involves finding a donor. Doctors perform HLA typing on the patient and close relatives, as siblings have about a 25% chance of being a perfect match. If no match is found in the family, the search continues in national and international donor registries for a matched unrelated donor (MUD).

Stage 2: Conditioning Regimen
Once a donor is secured (if needed) and the patient is cleared for transplant, the conditioning phase begins. This is often the most intensive part of the process. The conditioning regimen consists of high-dose chemotherapy and/or total body irradiation, administered over several days. The American Cancer Society outlines its three primary goals:
- Destroy any remaining cancer cells in the body.
- Suppress the patient’s immune system to prevent it from rejecting the new donor cells (in allogeneic transplants).
- Make space in the bone marrow for the incoming healthy stem cells to engraft.
The specific drugs and radiation doses are tailored to each patient’s disease, age, and overall health. While highly effective, this phase is challenging and comes with significant side effects like nausea, fatigue, hair loss, and mouth sores (mucositis), all of which are proactively managed by the medical team with supportive care and medications.

Stage 3: Stem Cell Processing and Preparation
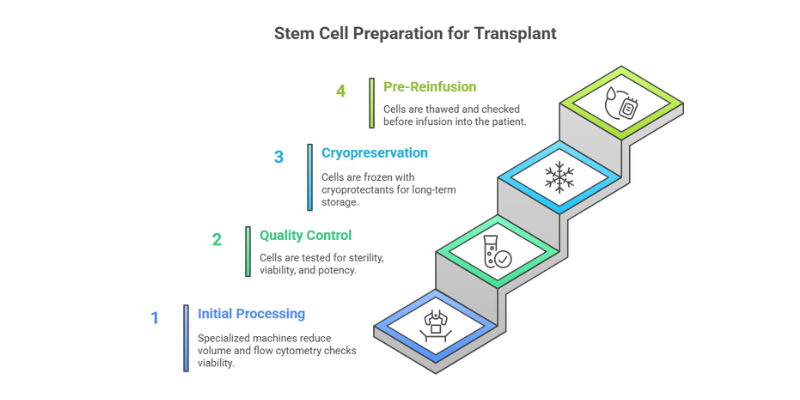
Before the infusion on transplant day, the collected stem cells go through a careful preparation process to ensure their safety and effectiveness:
- Initial Processing and Separation: Specialized machines (like Sepax or COBE 2991) reduce the collection volume. Flow cytometry is used to count cells and check their viability. In some cases, additional steps like T-cell depletion or tumor cell purging are performed for added safety.
- Quality Control Testing: The cells are tested to confirm sterility, viability, and potency. This includes CD34+ cell counts (a marker of stem cells) and colony-forming unit assays to ensure they can generate new blood cells.
- Cryopreservation: To keep cells safe until needed, cryoprotectants such as DMSO are added, and the cells are frozen using controlled-rate techniques. They are then stored long-term in liquid nitrogen tanks.
- Pre-Reinfusion Processing: When it’s time for transplant, the cells are carefully thawed, DMSO is reduced or removed if necessary, and final quality checks are performed. The stem cells are then ready for infusion into the patient — a pivotal step toward rebuilding a healthy blood system.
Stage 4: The Transplant Day (Day Zero): Infusion of Life
Day Zero – Stem Cell Infusion: This is the pivotal moment of a bone marrow transplant (BMT). A day or two after the conditioning therapy, the patient receives the new stem cells. The process is simple and painless, much like a blood transfusion. A bag of stem cells, similar in appearance to a unit of blood, is connected to the patient’s central line and infused slowly over a few hours while they remain awake under close monitoring. There is no surgery involved. Once infused, the cells travel to the bone marrow, where they begin rebuilding a healthy blood and immune system.
A patient holds up the bag of stem cells during the infusion process on transplant day, a pivotal moment in the BMT journey
Stage 5: Engraftment – The Critical Waiting Period
Following the infusion, the patient enters the engraftment phase. This is a period of waiting and watching as the new stem cells travel to the bone marrow, “take root,” and slowly begin to produce new, healthy blood cells. This critical process typically takes two to four weeks. During this time, the patient’s blood counts are at their lowest, leaving them highly vulnerable to infection and bleeding. Patients are cared for in specialized BMT units, often in positive-pressure isolation rooms with HEPA filtration to minimize exposure to germs. The medical team provides intensive supportive care, including antibiotics, blood and platelet transfusions, and vigilant monitoring for any signs of complications. The first sign of successful engraftment is a steady rise in the white blood cell count.
Stage 6: Post-Engraftment & Initial Recovery
Once engraftment is confirmed and blood counts reach a safe and stable level, the initial recovery phase begins. The focus shifts to managing any lingering side effects, monitoring for early complications like Graft-versus-Host Disease (GVHD), and gradually weaning the patient off intravenous medications and nutrition. This phase continues in the hospital until the patient is strong enough for discharge, which can be several weeks after the transplant. Even after discharge, patients are required to stay close to the transplant center for frequent follow-up appointments and monitoring for several months.
Why India? The Premier Destination for Bone Marrow Transplants
India has become a global leader in advanced healthcare, especially in complex procedures like bone marrow transplantation. For both international patients and those within the country, India offers a powerful advantage: world-class medical expertise, modern technology, and internationally renowned specialists — all at a fraction of the cost compared to many Western nations. This is not “cheap” healthcare, but rather accessible, high-quality treatment that combines excellence with affordability.
A. Comprehensive Cost Analysis: High-Quality Care Without the Financial Burden
India has emerged as one of the most affordable destinations for bone marrow transplants (BMT), offering world-class care at a fraction of the cost compared to the US or UK. According to Cancer Rounds, the average cost of a bone marrow transplant in India ranges between ₹15 lakh to ₹40 lakh (approximately $18,000 to $50,000), depending on the type of transplant, hospital, and patient’s condition.
- Autologous BMT: Around ₹15–20 lakh
- Allogeneic BMT (related donor): Around ₹25–30 lakh
- Allogeneic BMT (unrelated donor or haploidentical): Around ₹35–40 lakh
These costs generally include hospital stay, pre-transplant evaluation, chemotherapy or conditioning regimen, the transplant procedure, and immediate post-transplant care.
In comparison, the same procedure in Western countries can easily exceed $200,000–$250,000, highlighting India’s cost advantage without compromising on medical expertise or infrastructure.
By choosing India for treatment, patients not only benefit from high-quality healthcare and globally trained specialists, but also significantly reduce the financial burden of this life-saving procedure.
For more details, you can read the full cost breakdown at Cancer Rounds.
This cost advantage allows patients to access life-saving treatment that might otherwise be out of reach. The table below, compiled from various Indian medical tourism and hospital sources, provides an estimated cost comparison.
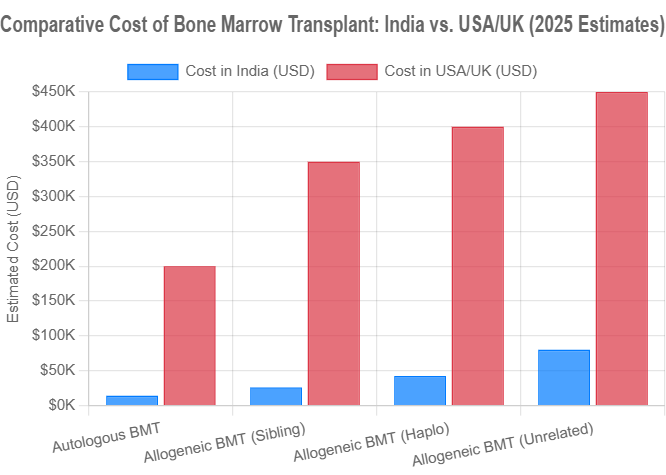
Data compiled from sources including Cancer Rounds and Flymedi.
It’s important to note that the final cost can be influenced by several factors:
- Hospital and City: Costs may vary slightly between major metropolitan hubs like Delhi, Mumbai, and Gurgaon.
- Patient’s Condition: The patient’s age, overall health, and the development of any post-transplant complications can extend the hospital stay and increase costs.
- Room Type: The choice of a private room versus a semi-private room will affect the final bill.
- Donor Type: As seen in the chart, transplants using unrelated or haploidentical donors are more complex and therefore more expensive than those using a patient’s own cells or a matched sibling’s.
B. Uncompromising Quality & High Success Rates
India’s cost advantage is matched by world-class quality. Leading hospitals have invested in advanced infrastructure and follow strict global standards. Many are accredited by JCI and NABH, recognized benchmarks for patient safety and care. Centers like BLK-Max and Fortis hold these accreditations, ensuring treatment on par with the best worldwide.
Success rates for BMT in India are comparable to international benchmarks, generally ranging from 60% to 90%. The outcome depends on many variables, including the specific disease, patient’s age, and transplant type. Some reports cite this high success rate as a key factor in India’s reputation. This success is driven by the adoption of advanced technology:
- Advanced Donor Matching: Use of high-resolution HLA typing to find the best possible donor match, which reduces the risk of complications like GVHD.
- Superior Infection Control: State-of-the-art BMT units with HEPA-filtered, positive-pressure isolation rooms to protect immunocompromised patients. The Hindu reports that these stringent protocols have significantly reduced post-transplant complications.
- Emerging Therapies: Leading Indian centers are at the forefront of research and are beginning to offer next-generation treatments like CAR-T cell therapy, further expanding treatment options for patients with relapsed cancers.
A state-of-the-art BMT unit room in an Indian hospital, featuring advanced infrastructure and amenities for patient comfort and safety
C. Top Hospitals and Renowned Specialists: A Spotlight on Excellence
India is home to a cadre of internationally trained and highly experienced hematologists and BMT specialists. The Delhi-National Capital Region (NCR), in particular, has become a major destination for medical tourists due to its concentration of world-class hospitals. Here is a look at some of the leading institutions:
| Hospital | Location | Key Strengths & Facts | Notable Doctors Mentioned |
|---|---|---|---|
| Fortis Memorial Research Institute (FMRI) | Gurgaon | JCI & NABH accredited. Runs one of India’s largest BMT programs, having completed over 1000 transplants. Known for expertise in transplants for Multiple Sclerosis and Thalassemia. A ‘Mecca of Healthcare’ for the Asia Pacific region. | Dr. Rahul Bhargava, Dr. Vikas Dua |
| BLK-Max Super Speciality Hospital | New Delhi | Considered one of the largest BMT centers in Asia, with over 800 successful transplants. Pioneered the first unrelated donor transplant for Thalassemia in Delhi. Features ultra-modern infrastructure and an internationally trained faculty. | Dr. Dharma Choudhary, Dr. Sanjeev Kumar |
| Indraprastha Apollo Hospitals | New Delhi | A JCI-accredited, 710+ bed tertiary care hospital. The BMT unit has performed over 500 transplants with excellent success rates and is known for its stringent infection control protocols. Offers 52 specialties under one roof. | Dr. Shishir Seth |
| Medanta – The Medicity | Gurgaon | NABH & NABL accredited, founded by world-renowned surgeon Dr. Naresh Trehan. Features a comprehensive Cancer Institute with a robust and highly respected BMT unit. A multi-speciality institute with 1600 beds. | (Team of experts) |
The Road to Recovery: A Marathon, Not a Sprint
The transplant day is only the beginning of recovery. Healing after a bone marrow transplant is a gradual journey that demands patience, resilience, and strong support. It is best seen as a marathon, not a sprint, with the aim of returning to a healthy, active life. While timelines vary, full recovery often takes up to a year or longer. According to Narayana Health, the duration depends on several individual factors.
The First 100 Days: The Most Critical Phase
The first 100 days after transplant are the most critical. During this time, the new immune system is still developing, leaving patients highly vulnerable to infections and complications. Doctors focus on close monitoring and proactive care, with frequent check-ups, blood tests, and supportive treatments. Patients often need to stay in or near the hospital to manage risks and ensure the graft is working properly.
Long-Term Recovery (Up to a Year and Beyond)
After the first 100 days, recovery continues at a steady pace. The immune system gradually rebuilds its strength, a process that can take many months. This phase involves significant lifestyle adjustments to support the healing body:
- Nutrition and Diet: A balanced diet is vital for recovery. Dietitians help patients design meal plans that support healing, manage weight, and ease side effects. Strict food safety practices are essential to reduce the risk of infections while the immune system remains weak.
- Physical Activity: Gradual reintroduction of light exercise helps rebuild strength, increase endurance, and improve overall well-being.
- Emotional and Psychological Support: A bone marrow transplant can be emotionally challenging for both patients and families. Studies from the Fred Hutchinson Cancer Center show that caregivers also face high stress, with about 1 in 5 reporting reduced quality of life. Support from counselors, patient groups, and loved ones plays a vital role in recovery and overall well-being.
Compassionate care from nurses and a strong support system are vital during the long recovery after a bone marrow transplant
For deeper insights on coping with the emotional and mental challenges after treatment, explore our guide on life after cancer and rebuilding mental health
Understanding the Risks and Side Effects
While a bone marrow transplant can be life-saving, it is also a complex treatment with potential risks. Patients and families should approach these challenges with awareness, not fear, so they are better prepared for the journey. The specific risks depend on factors such as the type of transplant, the patient’s age and health, and the condition being treated.
Short-Term Side Effects
Most short-term side effects come from the conditioning treatment (chemotherapy and radiation) and the low blood counts before engraftment. These effects are usually temporary and can be managed with supportive care:
- Nausea, Vomiting, and Diarrhea: Very common side effects managed with anti-nausea medications and hydration.
- Mucositis: Painful sores and inflammation in the mouth and throat, managed with pain relief and special mouthwashes.
- Fatigue and Weakness: A profound sense of tiredness is almost universal as the body works to recover.
- Hair Loss: A common and expected side effect of high-dose chemotherapy.
- Infection and Bleeding: The highest risk occurs during the pre-engraftment phase when white blood cell and platelet counts are extremely low. This is managed with antibiotics and transfusions. Cancer Research UK emphasizes that infection is a major risk during this period.
Potential Long-Term Complications
Some complications can arise months or even years after the transplant. These require long-term monitoring.
- Graft-versus-Host Disease (GVHD): A complication unique to allogeneic transplants, GVHD happens when the donor’s immune cells see the patient’s body as foreign and attack it. It may appear soon after transplant (acute) or later (chronic), often affecting the skin, liver, or gut. Treatment usually involves immunosuppressive drugs. Although a risk, this reaction can sometimes provide a helpful anti-cancer effect.
- Organ Damage: The intensive conditioning regimen can sometimes have long-term effects on organs like the liver, lungs, kidneys, or heart.
- Infertility: High-dose chemotherapy and radiation often cause permanent infertility. This is a significant quality-of-life issue, and patients are strongly encouraged to discuss fertility preservation options (sperm banking or egg freezing) with their medical team *before* starting treatment.
- Cataracts: Clouding of the lens of the eye can occur, particularly in patients who received total body irradiation.
- Secondary Cancers: There is a small but increased risk of developing a new type of cancer years after the transplant. Regular long-term follow-up and cancer screenings are essential.
Patient Stories: Voices of Hope
Behind the statistics and medical terminology are the powerful human stories of resilience, courage, and hope. These personal accounts provide invaluable perspective and inspiration for those embarking on the BMT journey.
A Caregiver’s Perspective: The Journey with Maddie
The family of Maddie, a young girl who battled a high-risk form of leukemia, shares their experience. They describe the “abject fear, the ceaseless praying and the nearly maniacal focus on providing for your child’s every comfort.” Her journey involved an urgent BMT at Texas Children’s Hospital after finding a perfect match through the Be the Match registry. They recount the grueling preparation, the “anticlimactic” but life-giving infusion, and the difficult recovery period, including severe complications that were expertly managed by her medical team. Today, Maddie is a thriving 10-year-old. Her family’s story is a testament to the dedication of medical teams and the selflessness of anonymous donors. “Each day, we give thanks… to all the skilled, kind staff… who work tirelessly to help their Maddies continue wonderful and meaningful lives.” (Source: Texas Children’s Hospital)
A Survivor’s Look Back: 30 Years After Transplant
Mike Rubin, who received a then-experimental bone marrow transplant 30 years ago at the Fred Hutchinson Cancer Center, reflects on his journey. He emphasizes the crucial role of his family, his “constellation of support,” which included his mother who acted as his primary caregiver and kept a journal to process the emotional turmoil. His story highlights that the road to wellness is not always easy, but a cure is possible. Now, 30 years later, he celebrates his survivorship and pays it forward to help others on the same path. (Source: Fred Hutchinson Cancer Center)
Frequently Asked Questions (FAQs)
Q1: Is the bone marrow transplant procedure itself painful?
This is a very common concern. The infusion of the stem cells on “Day Zero” is not painful. It is administered through a central line, much like a blood transfusion, and the patient is awake throughout. However, the preparatory conditioning regimen, which involves high-dose chemotherapy and/or radiation, can cause significant discomfort and side effects. These can include nausea, mouth sores (mucositis), and fatigue. It is important to know that your medical team will be working proactively to manage these side effects with a range of medications and supportive care to keep you as comfortable as possible.
Q2: What is the success rate of BMT in India?
The success rates for bone marrow transplants in India are high and are comparable to those of leading medical centers worldwide. Generally, success rates range from 60% to 90%. Some reports from 2024 indicate success rates as high as 85-90%. However, “success” is a complex term. The exact rate depends heavily on several factors: the specific disease being treated, the stage of the disease, the patient’s age and overall health, the type of transplant (autologous, allogeneic, etc.), and the expertise of the transplant center. It is best to discuss your individual prognosis with your transplant physician.
Q3: How do you find a BMT donor?
For an allogeneic transplant, the search for a donor is a critical step. The process begins with the patient’s immediate family. Siblings are tested first, as they have a 1 in 4 chance of being a perfect HLA (Human Leukocyte Antigen) match. If a suitable match is not found within the family, the search expands to national and international donor registries. In India, organizations like the DATRI Blood Stem Cell Donors Registry maintain a database of volunteer donors. The development of haploidentical (half-match) transplants has been a major breakthrough, as it means most patients can find a suitable donor in a parent, child, or sibling. Finding a perfect match is a key risk and challenge in allogeneic transplants.
Q4: What is the age limit for a bone marrow transplant?
There is no strict chronological age limit for a BMT. Eligibility is determined more by a patient’s “physiologic age”—their overall health, fitness, and the function of their major organs. In the past, BMT was typically reserved for younger patients. However, the development of reduced-intensity conditioning (RIC) regimens, which use lower doses of chemotherapy, has made transplants a safe and effective option for older patients. According to BLK-Max Hospital, transplants can be performed on patients up to 70 years of age, though this is always assessed on a case-by-case basis by the BMT physician.
Conclusion: Your Path to a Healthier Future
A bone marrow transplant is one of the most complex yet transformative treatments in modern medicine. It offers the possibility of cure and a return to a full life for those facing serious diseases. India has emerged as a global hub for this procedure, combining internationally accredited hospitals, skilled specialists, advanced technology, and accessible costs.
The journey requires courage, knowledge, and strong support. By understanding the process, recovery, and risks — and by choosing the right medical team — patients and families can move forward with greater confidence. It is a marathon, but with the right care, it is a race that can be won.
Key Takeaways
- BMT is a System Reboot: It replaces a diseased blood-cell factory with a healthy one via an infusion, not major surgery.
- India Offers Affordable Excellence: Patients can save 50-70% on costs compared to the West, without compromising on care at JCI-accredited hospitals.
- The Procedure is a Multi-Stage Journey: It involves evaluation, conditioning, the transplant day, and a critical engraftment period.
- Recovery is a Marathon: Full recovery takes a year or more, with the first 100 days being the most critical. Emotional and family support is vital.
- Knowledge is Power: Understanding the risks, such as GVHD and infection, allows for better preparation and management.
If you or a loved one are considering a bone marrow transplant and are exploring options in India, taking the first step is crucial. We encourage you to reach out to the international patient services department of a leading, accredited hospital. They can provide a no-obligation second opinion, a detailed treatment plan, and a cost estimate based on your specific medical records.
Have you or a family member been through a BMT journey in India? Share your experience or ask questions in the comments below. Your story could provide invaluable hope and insight to others in our community.
Medical Disclaimer
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before making medical decisions.
