I. Introduction: The Dawn of a New Era in Cancer Care
Cancer remains one of humanity’s most formidable health challenges. In the ongoing battle against this disease, radiotherapy has emerged as a cornerstone of modern treatment. Linear Accelerator (LINAC) technology has revolutionized external beam radiotherapy, transforming it from a relatively blunt instrument into a highly sophisticated and targeted therapy.
“The medical linear accelerator (linac) is the primary workhorse for radiation oncology,” states Oncology Medical Physics. This article explores LINAC technology: what it is, how it works, its key components, clinical applications, and future innovations.
II. How LINACs Work: The Core Technology
Defining LINAC: More Than Just a Machine
A Linear Accelerator (LINAC) is a sophisticated device that uses high-frequency electromagnetic waves to accelerate charged particles to high energies along a straight path. In medicine, LINACs generate precisely controlled beams of X-rays or electrons for cancer treatment. The International Atomic Energy Agency explains that a LINAC “uses electricity to generate high energy beams of X-rays or electrons,” which are directed at tumors to destroy cancer cells.
The Journey of a Particle: From Generation to Therapeutic Beam
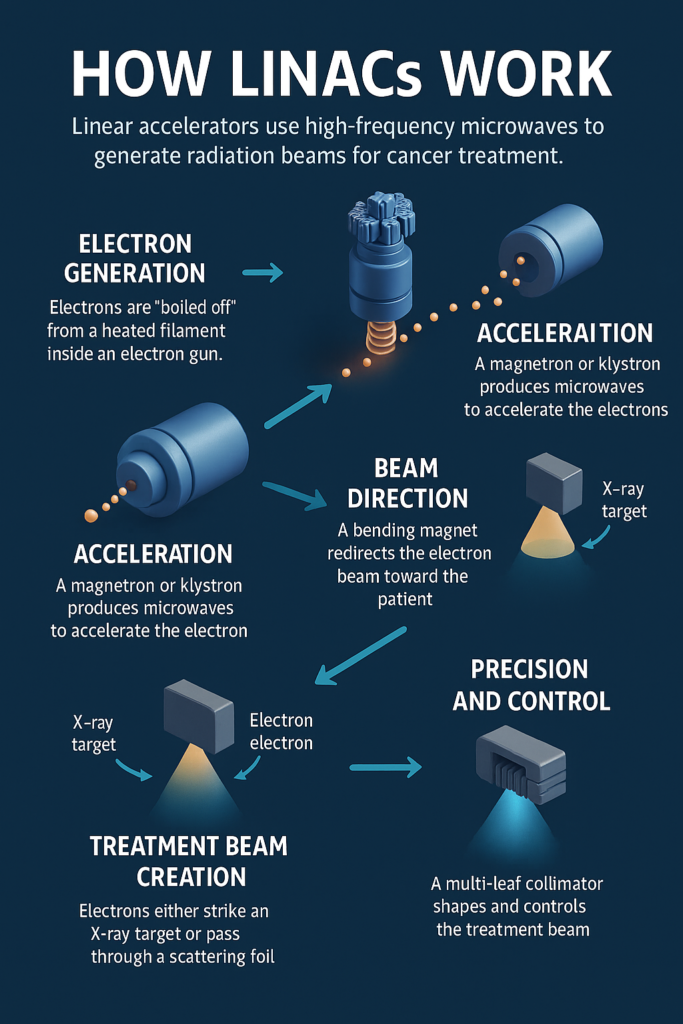
The process of generating radiation in a LINAC follows these key steps:
- Electron Generation: The journey begins in the electron gun where a heated filament “boils off” electrons through thermionic emission.
- Acceleration: A powerful microwave generator (Klystron or Magnetron) produces high-power radiofrequency waves fed into the accelerating waveguide. Electrons effectively “ride” these waves, gaining energy as they travel.
- Beam Direction: Once accelerated, a bending magnet redirects the electron beam from the horizontal accelerating waveguide toward the treatment area.
- Treatment Beam Creation: For deep tumors, electrons strike a tungsten target to produce X-rays. For superficial tumors, the electron beam passes through a scattering foil to create a uniform treatment beam.
Precision and Control: The Hallmarks of Modern LINACs
Modern LINACs offer remarkable precision through:
- Energy Selection: Various X-ray and electron beam energies allow customized treatment based on tumor depth.
- Beam Shaping: Several components contribute to precise targeting:
- Collimators: Heavy metal blocks that define the radiation field size.
- Multi-Leaf Collimator (MLC): Computer-controlled metal “leaves” that create a beam shape conforming precisely to the tumor’s complex outline.
- Flattening Filters: Create uniform dose distribution across the treatment field.
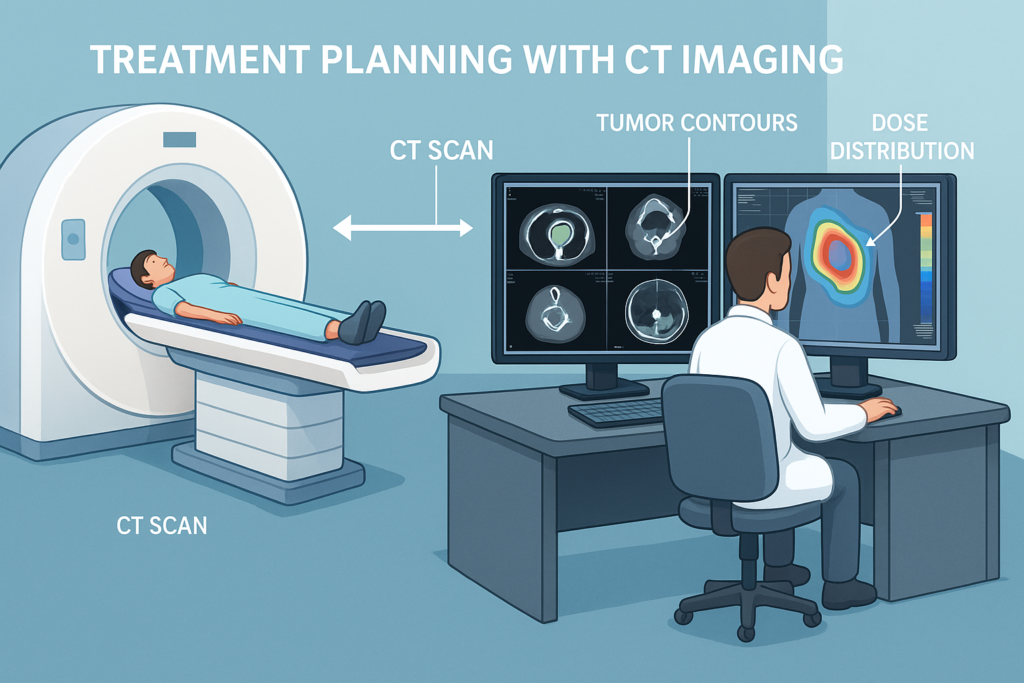
Accurate imaging is crucial in ensuring the success of LINAC-based radiation therapy. Before treatment begins, patients often undergo a CT scan to map the exact size, shape, and location of the tumor. This imaging data helps clinicians develop highly targeted radiation plans. If you’re curious about how CT scans work and their role in medical diagnostics, check out our detailed guide on CT Scan Machine: A Complete Guide for Professionals & Enthusiasts
Key Takeaways: How LINACs Work
- LINACs accelerate electrons to high energies using microwaves in a linear waveguide.
- These electrons either produce X-rays for deep tumors or are scattered to treat superficial tumors directly.
- Precision is achieved through energy selection and sophisticated beam shaping with Multi-Leaf Collimators.
III. The Heart of LINAC: Key Components and Their Roles
A medical LINAC is composed of several sophisticated subsystems working together to deliver precise radiation therapy:
Beam Generation and Acceleration
- Electron Gun: The source of electrons, consisting of a heated filament that “boils off” electrons which are immediately accelerated.
- RF Power Source: Klystrons (higher energy) or Magnetrons (lower energy) generate microwaves that power the acceleration process.
- Accelerating Waveguide: A specialized tube with resonant cavities where electrons gain energy from microwave fields as they travel.
- Bending Magnet: Redirects the high-energy electron beam toward the patient, typically at 90° or 270°.
Beam Shaping and Delivery (Treatment Head)
- Target/Scattering Foils: Tungsten target for X-ray production or foils that spread electron beams for uniform field coverage.
- Primary Collimator: Fixed opening that initially shapes the beam.
- Flattening Filter: Cone-shaped metal that creates uniform X-ray intensity across the treatment field.
- Ionization Chambers: Monitor radiation dose rate and total dose for safety and accuracy.
- Secondary Collimators: Movable heavy metal blocks defining rectangular field shapes.
- Multi-Leaf Collimator (MLC): Independently controlled tungsten “leaves” allowing complex beam shaping.
Patient Support and Imaging
- Treatment Couch: Precise positioning system with multiple degrees of freedom.
- Gantry: Rotating structure housing the accelerator components, enabling treatment from any angle around the patient.
- Image Guidance Systems: Essential for position verification, including Electronic Portal Imaging Device (EPID) and On-Board kV Imaging System for 2D images or 3D Cone-Beam CT.
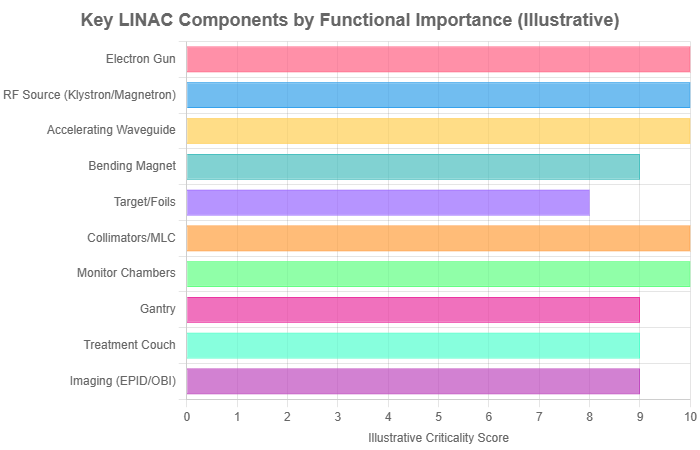
Illustrative chart showing key LINAC components. Actual system complexity involves deep interplay between all parts.
IV. A Brief History: The Evolution of LINAC Technology
The medical LINAC’s journey began in 1953, when the first treatment was delivered in London, UK. In 1956, at Stanford University, Dr. Henry Kaplan and collaborators adapted a linear accelerator for cancer treatment. Stanford Medicine News notes, “In the 50 years since Henry Kaplan developed the first medical linear accelerator at Stanford, it has become the backbone of radiation therapy for cancer worldwide.”
Technological evolution followed with improvements in beam energy and stability, integration of computer control, development of Multi-Leaf Collimators (MLCs) for precise beam shaping, and incorporation of advanced imaging systems. These advancements enabled sophisticated treatment techniques like Intensity-Modulated Radiation Therapy (IMRT), Volumetric Modulated Arc Therapy (VMAT), and Stereotactic Radiosurgery (SRS).
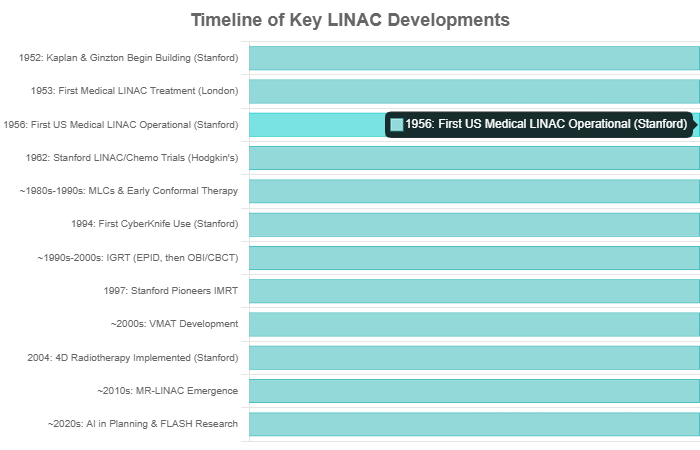
Timeline illustrating key milestones in LINAC technology development.
Key Historical Milestones
- 1953: First patient treated with a medical LINAC in London.
- 1956: Dr. Henry Kaplan’s team uses LINAC for cancer therapy at Stanford.
- 1980s-1990s: Multi-Leaf Collimators enable precise beam shaping.
- 1990s-2000s: Advanced imaging and IMRT/VMAT techniques enhance precision.
V. LINAC in Clinical Practice: Treating Cancer with Precision
The Treatment Planning Process
- Consultation: Radiation oncologist evaluates the patient and discusses treatment options.
- Simulation: Custom immobilization devices are created, and CT scans are performed with the patient in treatment position. MRI and PET scans may be added for better tumor visualization.
- Target Delineation: Oncologist outlines tumor volumes and nearby organs at risk (OARs) on imaging.
- Plan Optimization: Medical physicists and dosimetrists develop a treatment plan with optimal beam arrangements to deliver the prescribed dose while sparing healthy tissues.
- Quality Assurance: The plan undergoes rigorous verification before treatment begins.
The Treatment Delivery
- Patient Setup: Therapists position the patient precisely using immobilization devices and alignment lasers.
- Image Guidance: Pre-treatment imaging verifies target position, with adjustments made if necessary.
- Beam Delivery: The LINAC delivers radiation as planned, with the gantry potentially rotating to multiple angles.
- Fractionation: Treatment is typically delivered over multiple sessions (fractions) allowing healthy tissue to recover between treatments.
Common Cancers Treated with LINAC
LINAC radiotherapy effectively treats numerous cancers including brain tumors, head and neck cancers, lung cancer, breast cancer, prostate cancer, and liver cancer. Mercy.net notes that LINACs can treat “cancers of the brain, spine, head and neck, lung, breast, esophagus, stomach, rectum, uterus, prostate, bladder, liver and bones.”
Advanced LINAC Treatment Techniques
- 3D Conformal Radiotherapy (3D-CRT): Shapes beams to match the tumor’s general outline.
- Intensity-Modulated Radiation Therapy (IMRT): Varies beam intensity across small segments for highly conformal dose distribution.
- Volumetric Modulated Arc Therapy (VMAT): Delivers radiation while the LINAC rotates continuously around the patient with dynamically changing MLC positions.
- Image-Guided Radiation Therapy (IGRT): Integrates imaging before and during treatment for precise targeting.
- Stereotactic Radiosurgery (SRS) & Stereotactic Body Radiation Therapy (SBRT): Deliver high doses of precisely targeted radiation to small lesions in few treatment sessions.
Key Points in Clinical Practice
- Multidisciplinary Approach: Oncologists, physicists, dosimetrists, and therapists collaborate.
- Precision Planning: Detailed imaging, target delineation, and computational optimization.
- Image Guidance: Daily verification ensures accurate treatment delivery.
- Multiple Techniques: Various approaches tailored to specific cancer types and locations.
VI. The Cutting Edge and Future Horizons of LINAC Technology
LINAC technology continues to advance rapidly, with several breakthrough developments reshaping radiation oncology:
MR-LINAC: Real-time Soft-Tissue Visualization
MR-LINAC combines a Magnetic Resonance Imaging (MRI) scanner with a linear accelerator, providing superior soft-tissue visualization during treatment. A review in Frontiers in Oncology calls it “a major advance in image guided radiation technology.” This integration enables real-time tumor tracking and adaptive radiotherapy, particularly valuable for mobile tumors or those difficult to visualize with conventional imaging.
AI and Automation in Radiotherapy
Artificial intelligence is revolutionizing LINAC therapy through:
- Automated contouring of tumors and organs-at-risk
- Faster, more optimized treatment planning
- Enhanced quality assurance and error prediction
- Real-time adaptive adjustments during treatment
FLASH Radiotherapy: Ultra-High Dose Rates
FLASH radiotherapy delivers radiation at extremely high dose rates—over 40 Gray per second compared to conventional 0.1 Gy/s. Physics World reports on adapting LINACs to deliver radiation “at 300 Gy/s rather than 0.1 Gy/s.” Preclinical studies suggest this approach may significantly reduce damage to healthy tissues while maintaining tumor control.
Adaptive Radiotherapy and Personalization
Modern LINACs increasingly enable adaptive radiotherapy, modifying treatment plans during the course of therapy to account for anatomical changes. This approach is complemented by biologically-guided radiotherapy that aims to tailor radiation based on tumor biology rather than just anatomy, using functional imaging to identify radiation-resistant regions requiring higher doses.
Future Directions in LINAC Technology
- MR-LINAC: Real-time MRI guidance for superior soft-tissue targeting
- AI Integration: Automation of planning, delivery, and quality assurance
- FLASH Therapy: Ultra-high dose rates potentially reducing side effects
- Adaptive Approaches: Treatment plans that evolve with tumor changes
- Biology-Driven Treatment: Targeting based on tumor biological characteristics
VII. Benefits, Limitations, and Patient Experience
Key Benefits of LINAC Therapy
- Precision: Modern LINACs deliver radiation with millimeter accuracy, conforming to tumor shapes while sparing healthy tissue.
- Non-Invasive: Treatment requires no surgical incisions.
- Versatility: Effective for many cancer types and locations.
- Organ Preservation: Often maintains normal organ function that might be lost with surgery.
- Outpatient Treatment: Most patients continue normal activities during therapy.
Potential Side Effects and Limitations
Despite its precision, LINAC radiotherapy may cause side effects depending on treatment site, dose, and individual factors:
- Acute Side Effects: Temporary issues including fatigue, skin reactions, and site-specific effects (e.g., dry mouth for head/neck treatment, diarrhea for pelvic treatment).
- Late Effects: Potential long-term issues including tissue fibrosis, lymphedema, or organ dysfunction.
- Limitations: Not all cancers respond optimally to radiation; treatment typically requires multiple sessions over weeks; advanced systems may have limited availability in some regions.
Patient Journey and Side Effect Management
Effective management of the patient experience involves:
- Regular communication with the radiation oncology team
- Supportive care for symptom management
- Psychological support resources
- Long-term follow-up to monitor recovery and manage any late effects
Common Side Effects by Treatment Area
| Treatment Area | Common Side Effects | Management Approach |
| General | Fatigue, Skin Reactions | Rest, gentle skin care, moisturizers |
| Head & Neck | Mouth/throat soreness, dry mouth | Pain relief, mouth rinses, dietary modifications |
| Chest | Cough, shortness of breath | Cough suppressants, breathing exercises |
| Abdomen/Pelvis | Nausea, diarrhea, bladder irritation | Anti-emetics, anti-diarrheals, hydration |
VIII. Conclusion: LINAC’s Impact and Future
The medical linear accelerator represents a cornerstone of modern cancer care. From its early development in the 1950s to today’s sophisticated systems, LINAC technology has transformed radiotherapy through unprecedented precision, versatility, and effectiveness.
Current advances in MR-LINAC integration, artificial intelligence applications, and novel approaches like FLASH therapy promise to further enhance treatment precision, reduce side effects, and improve outcomes. These innovations build on the solid foundation of decades of scientific and clinical progress.
LINACs continue to play a vital role in treating millions of cancer patients worldwide, offering hope through non-invasive, effective therapy. As technology evolves, this life-saving tool will remain central to oncology’s arsenal, continually expanding the possibilities for cancer treatment and survivorship.
LINAC’s Impact Summarized
- Revolutionary Technology: Transformed radiation therapy through precision targeting
- Continuous Evolution: From basic machines to advanced systems enabling sophisticated techniques
- Clinical Versatility: Effective for diverse cancer types with multiple delivery methods
- Future Promise: Ongoing innovation through MR integration, AI, and novel approaches
- Patient Impact: Improved survival and quality of life for countless cancer patients
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.