A defibrillator is a medical device that saves lives by delivering a controlled electrical shock to the heart. This shock is not a “restart” button but a reset mechanism. It works by simultaneously depolarizing a critical mass of heart muscle cells, terminating chaotic electrical rhythms like ventricular fibrillation and allowing the heart’s natural pacemaker to re-establish a normal, effective beat.
Table of Contents
First Principles: The Heart’s Electrical System and Why It Fails
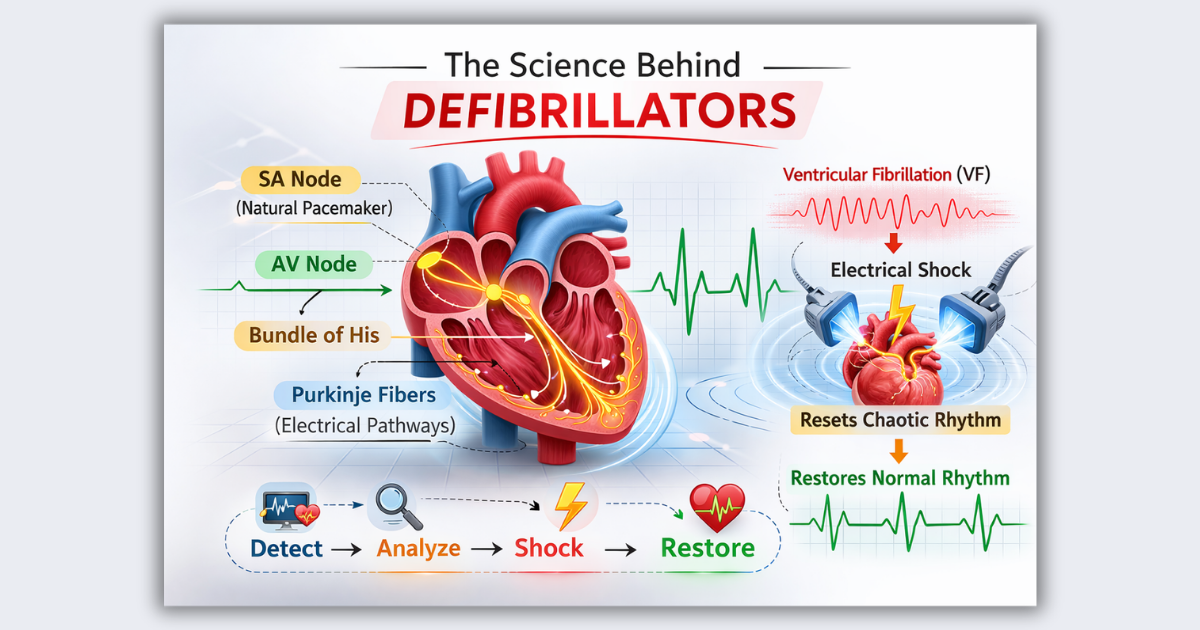
To understand how defibrillators work, we must first understand the heart’s own electrical system. The heart is not just a muscle; it’s an electro-mechanical pump, where electrical signals orchestrate its rhythmic contractions.
What is Normal Cardiac Electrical Activity?
In a healthy heart, a tiny cluster of cells called the sinoatrial (SA) node acts as the natural pacemaker. It generates a regular electrical impulse that travels through specialized conduction pathways across the atria (upper chambers) and then to the ventricles (lower chambers). This coordinated wave of depolarization causes the heart muscle to contract in a synchronized fashion, efficiently pumping blood to the body.
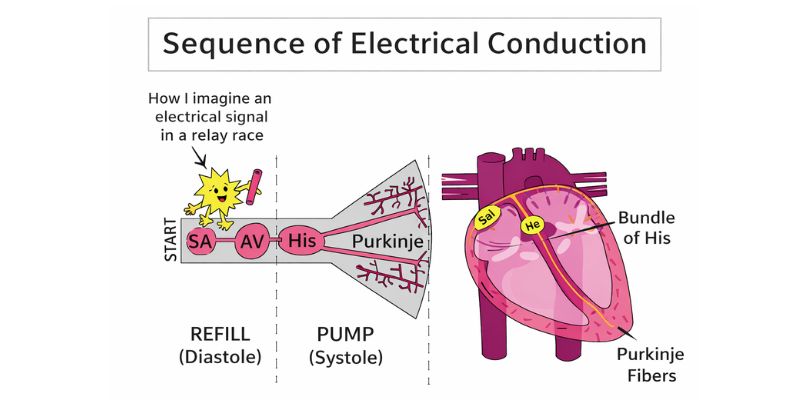
The heart’s intrinsic electrical conduction system, starting with the SA node, ensures a coordinated heartbeat.
Why Do Life-Threatening Arrhythmias Occur?
Sometimes, this orderly system breaks down. Conditions like a heart attack (myocardial infarction), severe electrolyte imbalances, or structural heart disease can damage heart tissue, creating irritable and unstable electrical pathways. This can lead to two primary shockable arrhythmias:
- Ventricular Tachycardia (VT): A very fast, but often regular, rhythm originating in the ventricles. If it’s too fast, the ventricles don’t have time to fill with blood, leading to a loss of pulse (pulseless VT).
- Ventricular Fibrillation (VF): The most serious arrhythmia. Instead of a single pacemaker, multiple chaotic electrical impulses fire randomly from the ventricles. This causes the heart muscle to quiver or “fibrillate” uselessly instead of contracting. No blood is pumped, leading to sudden cardiac arrest (SCA).
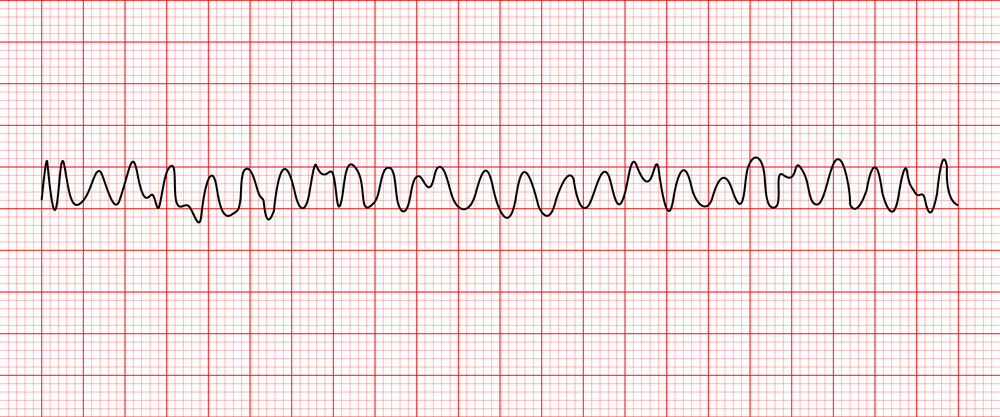
An electrocardiogram (ECG) showing the disorganized electrical waves of Ventricular Fibrillation, which results in no effective cardiac output.
Why Shock Therapy Works Scientifically
During VF, the heart’s electrical activity is like an orchestra without a conductor, with every musician playing a different tune. A defibrillation shock acts like a loud, powerful command that silences the entire orchestra at once. By delivering a strong electrical current, it forcibly depolarizes a large majority of the heart cells simultaneously. This abrupt electrical reset extinguishes the chaotic reentrant circuits, creating a momentary pause and allowing the SA node—the heart’s natural conductor—to regain control and re-establish a normal, organized rhythm (sinus rhythm).
The Physics Behind Defibrillation
The success of defibrillation hinges on delivering the right amount of electrical energy to the heart muscle. This involves a delicate interplay of voltage, current, energy, and the body’s own resistance.
Electrical Depolarization: The Cellular Reset
At a cellular level, heart muscle cells (myocytes) maintain an electrical charge difference across their membrane, known as the resting membrane potential. An electrical stimulus causes this potential to reverse, a process called depolarization, which triggers muscle contraction. A defibrillation shock provides a powerful external stimulus that depolarizes a critical mass of these cells all at once, including those that are stuck in chaotic firing patterns.
Voltage, Current, and Joules: The Trifecta of Defibrillation
These terms are often used interchangeably but have distinct meanings:
- Voltage (V): Think of this as the electrical “;pressure” or “push.” A defibrillator uses high voltage (often over 1,000 volts) to create a strong enough force to drive electricity through the chest.
- Current (A): This is the actual flow of electrons through the body and heart. It is the current, not the voltage, that depolarizes the heart cells. The goal is to get enough current to the heart muscle.
- Joules (J): This is the measure of energy delivered. Energy is a product of voltage, current, and time. Defibrillators are programmed in joules because it represents the total dose of therapy delivered. Typical adult doses for modern biphasic defibrillators range from 120 to 200 joules for an initial shock.
Transthoracic Impedance (TTI): The Body’s Resistance
The body is not a perfect conductor. Transthoracic impedance is the total resistance the chest presents to the flow of electrical current. Factors like chest size, hair, skin moisture, and electrode-to-skin contact influence TTI. A high TTI can reduce the amount of current reaching the heart, potentially making the shock ineffective. Defibrillator pads and conductive gel are designed to minimize this impedance.
Monophasic vs. Biphasic Waveforms
The “waveform” describes the direction of current flow during the shock. Early defibrillators used a monophasic waveform, where current flows in only one direction. Modern devices almost exclusively use biphasic waveforms.
A biphasic shock delivers current in one direction for a specified duration, then reverses polarity and flows in the opposite direction. Studies have shown that biphasic waveforms can achieve successful defibrillation at lower energy levels than monophasic shocks, which may reduce the risk of skin burns and heart muscle damage.
| Feature | Monophasic Waveform | Biphasic Waveform |
| Current Flow | One direction (from one pad to the other). | Two directions (flows one way, then reverses). |
| Energy Required | Higher (typically 360 Joules for adults). | Lower (typically 120-200 Joules for adults). |
| Efficacy | Effective, but less so than biphasic at equivalent or lower energies. | More effective at terminating VF, especially at lower energy levels. |
| Potential for Myocardial Damage | Higher risk due to higher energy delivery. | Lower risk due to lower energy and more efficient current delivery. |
| Modern Usage | Largely replaced in new devices. Found in older models. | The standard in virtually all modern external and internal defibrillators. |
What Happens Inside the Heart When a Defibrillator is Used?
The process of defibrillation is a dramatic, split-second event at the cellular level that aims to restore order from chaos.
Cellular-Level Explanation: Overwhelming the Chaos
When a defibrillator shock is delivered, the strong electric field passes through the heart. This field creates a voltage gradient across each myocyte. The ends of the cells facing the positive electrode (anode) become hyperpolarized, while the ends facing the negative electrode (cathode) become depolarized. If the depolarization is strong enough to reach the cell’s activation threshold, it triggers a new action potential, effectively “capturing” the cell and forcing it into a synchronized state with its neighbors.
Resetting Myocardial Electrical Chaos
The key to success is achieving this effect across a “critical mass” of the ventricular myocardium. By depolarizing a sufficient percentage of the heart muscle at the same instant, the shock eliminates the multiple, random wavefronts that sustain VF. The chaotic electrical activity is extinguished because there are no longer enough excitable cells to perpetuate the disorganized circuits.
The Refractory Period: A Window for the Pacemaker to Resume Control
Immediately after being depolarized by the shock, the heart cells enter a “refractory period.” During this brief window of time, they are unable to be stimulated again. This enforced silence is crucial. It prevents the immediate re-initiation of fibrillation and gives the heart’s natural pacemaker, the SA node, a chance to fire and propagate a normal, organized impulse. If the SA node is still viable, it will take over and restore a life-sustaining rhythm.
Types of Defibrillators: Same Science, Different Applications
While the core principle of electrical defibrillation remains the same, the technology is packaged into different devices for specific users and situations.
Manual External Defibrillator
Used by paramedics, nurses, and doctors, these devices require the operator to interpret the heart rhythm on an ECG screen, select the appropriate energy level (in joules), and manually trigger the shock. They offer maximum control for trained professionals in advanced life support (ALS) scenarios.
Automated External Defibrillator (AED)
AEDs are designed for use by bystanders and first responders with minimal training. An internal computer analyzes the patient’;s heart rhythm through the pads and determines if a shockable rhythm (VF or pulseless VT) is present. If so, it automatically charges and instructs the user to deliver a shock (or delivers it automatically in some models). Their widespread availability in public places is critical for improving survival from out-of-hospital cardiac arrest.
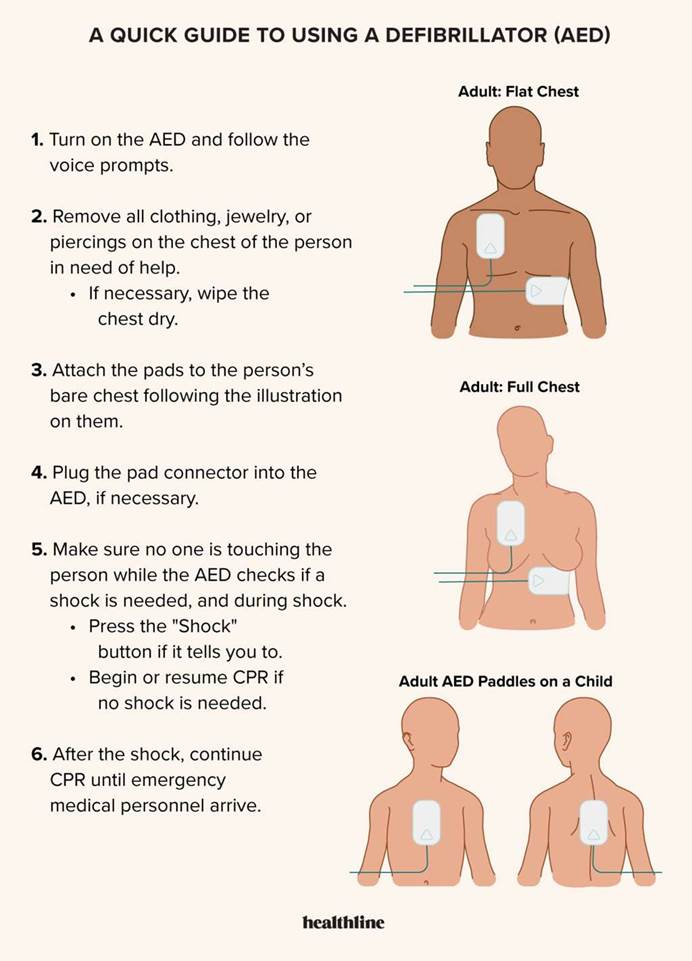
AEDs provide clear visual and voice prompts, including instructions for correct pad placement, making them usable by the general public.
Implantable Cardioverter-Defibrillator (ICD)
An ICD is a small, battery-powered device surgically implanted in the chest of patients at high risk for life-threatening arrhythmias. It continuously monitors the heart’;s rhythm. If it detects VF or VT, it automatically delivers a low- or high-energy shock directly to the heart muscle via wires (leads). It acts as a 24/7 guardian against sudden cardiac death.
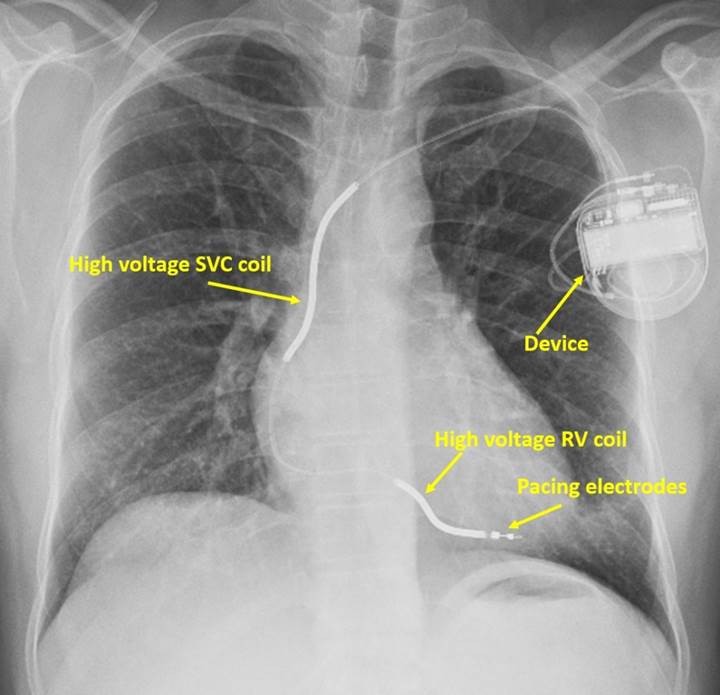
An ICD is implanted under the skin to provide constant monitoring and immediate treatment for dangerous arrhythmias.
Wearable Cardioverter-Defibrillator (WCD)
A WCD is a vest worn by patients at temporary high risk for SCA, such as after a major heart attack or while waiting for a heart transplant. It functions like an external AED, with sensors in the vest that monitor the heart. If a life-threatening arrhythmia is detected, the device delivers a shock through electrodes integrated into the vest. It provides a bridge of protection until a permanent solution like an ICD is viable or the risk subsides.
A Clinical Workflow Example: From Collapse to Shock
Imagine a person suddenly collapses in a public place. Here is how the science of defibrillation is applied in a real-world emergency:
1. Recognition and CPR: A bystander recognizes the signs of cardiac arrest (unresponsive, not breathing normally) and calls for emergency services. High-quality cardiopulmonary resuscitation (CPR) is started immediately to circulate oxygenated blood to the brain and heart.
2. AED Arrival and Application: Another bystander retrieves an AED. The device is turned on, and the pads are applied to the patient’s bare chest as shown in the device’s diagrams.
3. Rhythm Detection: The user stops CPR when prompted by the AED. The device’;s algorithm analyzes the heart’s electrical activity. It is specifically looking for the chaotic signature of VF or the rapid pattern of pulseless VT.
4. Energy Selection and Charging: The AED detects VF. It announces, “Shock advised,” and automatically charges its capacitor to a pre-programmed energy level (e.g., 150 Joules). It warns everyone to “stand clear.”
5. Shock Delivery: The user presses the flashing shock button. The stored electrical energy is discharged in a biphasic waveform through the pads, across the chest, and through the heart.
6. Outcome and Post-Shock Care: The shock successfully terminates the VF. The AED may prompt the user to resume CPR immediately to help the recovering heart circulate blood. The heart’s SA node begins to fire, and a normal rhythm is restored. Paramedics arrive to provide advanced care and transport the patient to the hospital.
Learn more about related cardiac support technologies like the IABP machine and how they work in tandem with defibrillators in critical care settings. IABP machine explained — working principle, uses & hemodynamics
Myth vs. Science: Debunking Common Defibrillator Misconceptions
Myth: A defibrillator “restarts” a heart that has flatlined.
Science: This is one of the biggest myths, perpetuated by television dramas. A defibrillator cannot shock asystole (a flatline), which represents a total absence of electrical activity. A shock is useless if there is no chaos to reset. The only treatment for asystole is high-quality CPR and medications in an attempt to generate a shockable rhythm.
Myth: You can accidentally shock and harm someone who doesn’t need it.
Science: This is virtually impossible with a modern AED. AEDs are “;automated” for a reason. Their internal computer will only advise a shock if it detects the specific electrical signature of VF or pulseless VT. If a person has a normal rhythm, is in asystole, or has a different non-shockable arrhythmia, the AED will state “No shock advised” and will not charge.
Myth: More energy is always better.
Science: While sufficient energy is crucial, excessive energy can cause skin burns and damage the heart muscle without increasing the chance of success. The goal is to use the lowest effective dose. Biphasic technology was a major advance because it allows for successful defibrillation at lower energy levels. Some protocols call for escalating energy levels for subsequent shocks if the first is unsuccessful, but the initial shock is carefully calibrated.
Frequently Asked Questions (FAQ)
How does a defibrillator work?
A defibrillator works by delivering a targeted electrical shock to a heart experiencing a life-threatening arrhythmia like ventricular fibrillation. This shock simultaneously depolarizes a large portion of the heart muscle, stopping the chaotic electrical activity and allowing the heart’s natural pacemaker to re-establish a normal, effective rhythm.
Why is ventricular fibrillation (VF) shockable but asystole (flatline) not?
VF is shockable because it is a state of disorganized electrical chaos. A shock can reset this chaos. Asystole is the absence of electrical activity. There is no rhythm to reset, so a shock would have no effect. The treatment for asystole is CPR and drugs to try and stimulate some electrical activity.
How much voltage does a defibrillator use?
An external defibrillator can generate a very high voltage, often between 1,000 and 2,000 volts, to overcome the body’s natural resistance (transthoracic impedance) and deliver sufficient current to the heart. However, the device’s setting is measured in joules (energy), not volts.
Is defibrillation safe for the rescuer and the patient?
Yes, when used correctly. AEDs have numerous safety features. They provide clear audio and visual prompts, including warnings to “stand clear” before a shock. They will not deliver a shock unless a shockable rhythm is detected. While the shock itself is a powerful intervention, the risk of not using a defibrillator during cardiac arrest is certain death.
Can an AED be used by someone who is not a doctor?
Absolutely. AEDs are specifically designed for use by the general public. They provide simple, step-by-step voice instructions to guide a lay rescuer through the entire process, from applying the pads to delivering a shock. No medical degree is required to save a life with an AED.
Key Takeaways
- Defibrillators treat life-threatening arrhythmias by delivering an electrical shock that resets the heart’s chaotic electrical activity.
- They do not “restart” a flatlined heart (asystole); they only work on shockable rhythms like Ventricular Fibrillation (VF) and pulseless Ventricular Tachycardia (VT).
- The key to success is delivering enough current to depolarize a critical mass of heart muscle, which is achieved by using high voltage to overcome the body’s impedance. The total dose is measured in joules.
- Modern defibrillators use biphasic waveforms, which are more effective at lower energy levels than older monophasic designs, potentially reducing heart muscle damage.
- Automated External Defibrillators (AEDs) are safe and designed for use by the public, analyzing the rhythm and only allowing a shock when necessary.
- Time is critical. For every minute that defibrillation is delayed, the chance of survival from SCA decreases by about 10%.
- Different types of defibrillators (Manual, AED, ICD, WCD) apply the same core science to different clinical scenarios and user groups.
A Note on the Future of Defibrillation
Defibrillation technology continues to evolve. Research is focused on smarter algorithms that can better predict and differentiate arrhythmias, personalized energy dosing based on patient impedance, and improved integration with CPR feedback devices. Innovations like drone-delivered AEDs aim to slash response times in rural areas. As our understanding of cardiac electrophysiology deepens, the defibrillator will remain a cornerstone of emergency medicine, becoming even safer, faster, and more effective at turning a life-ending event into a second chance.
Want to Go Deeper?
If you’d like to strengthen your understanding of cardiac electrical activity, ECG interpretation, and defibrillation science, these trusted resources are worth exploring:
Affiliate Disclosure:
Some links in this article may be affiliate links. If you purchase through them, I may earn a small commission at no extra cost to you. This helps support educational content on MedTechInsighter.