Unveiling the Invisible: An Introduction to Medical Imaging
Before the late 19th century, a physician’s understanding of the human body’s interior was limited to what could be gleaned from a physical examination, the sounds from a stethoscope, or, in dire circumstances, the revelations of exploratory surgery. The ability to see inside the body without making an incision was the stuff of science fiction. Today, medical imaging technologies have made non-invasive visualization the cornerstone of modern diagnostics, allowing us to detect disease, guide treatment, and understand human physiology with astonishing clarity.
A solid grasp of medical imaging technologies is no longer a niche skill reserved for radiologists. It is a vital competency for biomedical engineers designing the next generation of devices, clinicians making critical diagnostic decisions, students entering the multifaceted world of healthcare, and even patients who are increasingly empowered to understand their own care pathways. These technologies represent a powerful intersection of physics, engineering, computer science, and medicine.
This guide will provide a comprehensive exploration of the four pillars of modern medical imaging: X-ray, Computed Tomography (CT), Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET-CT). We will delve into their underlying scientific principles, explore their primary clinical applications, compare their strengths and weaknesses, and look ahead to the exciting future of a field dedicated to making the invisible visible.
The Four Pillars of Medical Imaging Technologies: A Detailed Breakdown
X-ray: The Foundation of Radiography
X-ray imaging, or radiography, is the original and still the most common form of medical imaging technologies. It utilizes a small, controlled dose of ionizing radiation to create two-dimensional images of the body’s internal structures. Its discovery in 1895 by German physicist Wilhelm Conrad Röntgen revolutionized medicine, providing the first-ever window into the living human body (NDE-Ed.org).
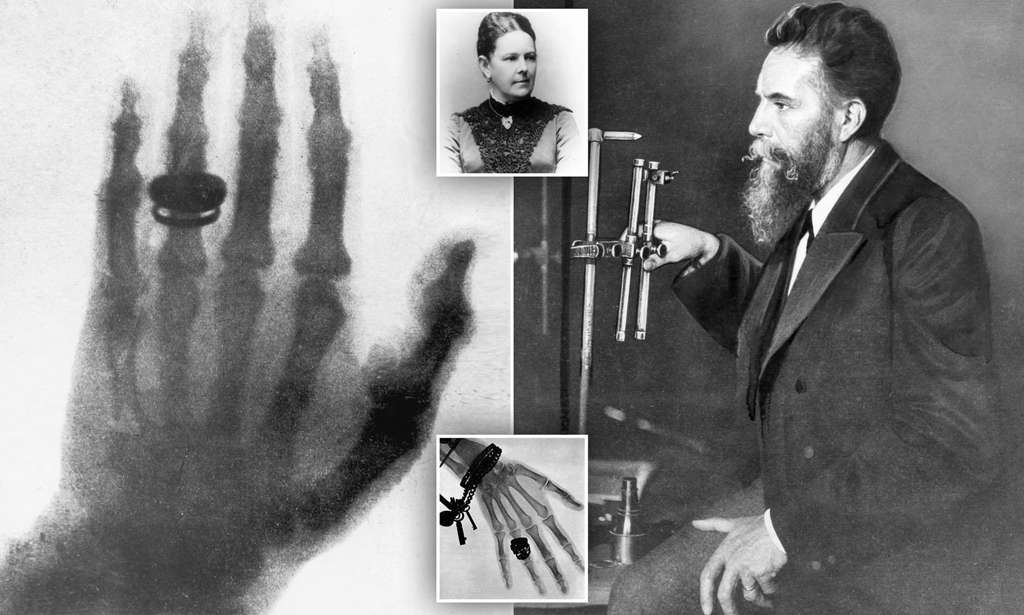
A composite image showing Wilhelm Röntgen and the first X-ray he took of his wife’s hand in 1895, revealing her bones and wedding ring
The Science Behind the Image (Technical Principles)
The function of X-ray technology, a core component of medical imaging technologies, is rooted in a principle known as differential attenuation. X-rays are a form of high-energy, short-wavelength electromagnetic radiation, similar to light but with enough energy to pass through many materials (Wikipedia). The process involves two key components: an X-ray tube that generates the radiation and a detector (traditionally film, now mostly digital) that captures the image.
- Differential Attenuation: When the X-ray beam passes through the body, different tissues absorb or “attenuate” the radiation to varying degrees. Dense tissues like bone absorb a significant amount of radiation, allowing very little to pass through to the detector. This results in these areas appearing white or light gray on the image.
- Tissue Penetration: Conversely, soft tissues such as muscle, fat, and organs are less dense and allow more X-rays to pass through, appearing as darker shades of gray. Air-filled spaces, like the lungs, absorb almost no radiation and appear black.
Primary Clinical Applications
Due to its speed, accessibility, and low cost, X-ray remains a first-line diagnostic tool for numerous conditions.
- Orthopedics: It is the gold standard for diagnosing bone fractures, dislocations, and evaluating joint abnormalities like arthritis (Cleveland Clinic).
- Chest Imaging: Essential for detecting conditions within the thoracic cavity, such as pneumonia, lung cancer, and cardiomegaly (an enlarged heart).
- Dentistry: Widely used to identify cavities, impacted teeth, and other dental and jaw issues.
- Mammography: A specialized, low-dose X-ray technique that is the primary screening tool for breast cancer.
Computed Tomography (CT): A 3D View with X-rays
Computed Tomography, commonly known as a CT or CAT scan, is an advanced technique within modern medical imaging technologies that builds upon fundamental X-ray principles. Instead of producing a single, flat image, a CT scanner acquires a series of X-ray images from many different angles around the body. A powerful computer then processes this data to create detailed cross-sectional “slices” and can even assemble them into three-dimensional models.

A medical professional operates a CT scanner while a patient lies on the scanner bed, with an observer in the control room
The Science Behind the Image (Technical Principles)
The ingenuity of the CT scanner, first invented by Sir Godfrey Hounsfield in 1972, lies in its mechanical and computational sophistication (MTMI). As one of the most significant advancements in medical imaging technologies, its core component is a donut-shaped structure called a gantry, which houses a rotating X-ray tube and an opposing arc of detectors.
- Rotational Acquisition: The patient lies on a bed that slowly moves through the gantry. As it moves, the X-ray tube rotates around the patient, continuously emitting a narrow beam of X-rays.
- Data Detection: Digital detectors on the opposite side of the gantry measure the X-ray attenuation profile from hundreds of different angles for each slice of the body.
- Tomographic Reconstruction: This vast amount of data is sent to a computer, which uses complex mathematical algorithms to reconstruct a detailed cross-sectional image. By stacking these slices, a 3D visualization can be created, offering a far more comprehensive view than a standard X-ray (NIBIB).
Primary Clinical Applications
The speed and detail of CT make it indispensable in many clinical scenarios, particularly in urgent situations.
- Trauma and Emergency Medicine: CT is the modality of choice for rapidly identifying internal injuries after an accident, including organ damage, internal bleeding, and complex bone fractures (OrthoInfo).
- Oncology: Crucial for detecting, staging (measuring size and location), and monitoring tumors throughout the body, especially in the chest, abdomen, and pelvis.
- Vascular Imaging (CTA): With the injection of an iodine-based contrast agent, CT Angiography (CTA) can visualize blood vessels to diagnose conditions like pulmonary embolisms (blood clots in the lungs), aneurysms, and vessel blockages.
- Complex Bone Issues: Provides detailed evaluation of intricate fractures (e.g., in the spine or pelvis) or small bony structures that are difficult to assess with a plain X-ray.
If you’re looking for a more in-depth understanding of how CT technology works in clinical settings, check out our complete guide to CT scan machines.
Magnetic Resonance Imaging (MRI): The Power of Magnets
Magnetic Resonance Imaging (MRI) is a sophisticated, non-invasive technology that stands apart from other medical imaging technologies like X-rays and CT scans because it does not use ionizing radiation. Instead, it leverages a powerful magnetic field, radio waves, and the natural properties of atoms in the body to generate exceptionally detailed images of soft tissues, organs, and other internal structures.
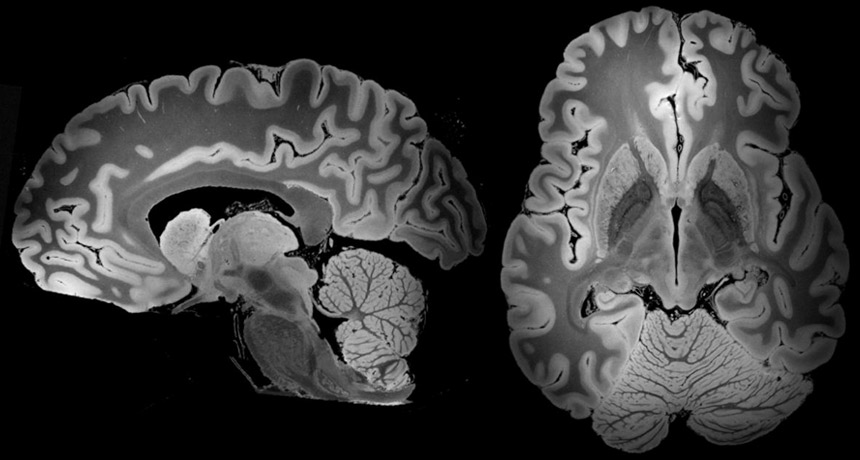
High-resolution sagittal and coronal MRI scans revealing the intricate soft tissue structures of the human brain
The Science Behind the Image (Technical Principles)
The physics of MRI, a key player among medical imaging technologies, is based on a phenomenon called Nuclear Magnetic Resonance (NMR). The process focuses on the behavior of protons—abundant in the water molecules of the human body—when placed in a strong magnetic field.
- Magnetization: The patient is placed inside the MRI scanner, which contains a powerful superconducting magnet (typically 1.5 to 3 Tesla). This strong magnetic field forces the body’s protons to align their rotational axes with the field (NIBIB).
- Excitation: A radiofrequency (RF) coil sends a pulse of radio waves into the patient. This pulse is tuned to the specific frequency of the protons, causing them to absorb energy and spin out of their alignment.
- Detection: When the RF pulse is turned off, the protons “relax” and realign with the magnetic field. As they do, they release the absorbed energy in the form of a faint signal, which is detected by the RF coils. The time it takes for protons to relax (T1 and T2 relaxation times) varies depending on the type of tissue they are in.
- Spatial Encoding: This is the key to forming an image. Smaller magnets, called gradient coils, are rapidly switched on and off to create slight variations in the magnetic field. This makes protons in different locations precess at slightly different frequencies, allowing the system to precisely map the origin of the detected signals and construct a detailed image (Wikipedia).
Primary Clinical Applications
MRI’s exceptional soft-tissue contrast makes it the superior choice for a wide range of diagnostic challenges.
- Neurology: Unmatched for imaging the brain and spinal cord. It is essential for detecting tumors, strokes, infections, and diagnosing degenerative conditions like multiple sclerosis.
- Musculoskeletal: The best modality for visualizing soft tissue injuries, including torn ligaments (e.g., ACL in the knee), tendon damage, and cartilage problems in joints.
- Oncology: Excellent for characterizing tumors in soft tissues (such as the brain, liver, and prostate) and assessing their response to treatment.
- Abdominal and Pelvic Imaging: Provides detailed evaluation of organs like the liver, kidneys, pancreas, and reproductive organs without radiation.
Positron Emission Tomography (PET-CT): Imaging Function, Not Just Form
Positron Emission Tomography (PET) is a type of nuclear medicine imaging that offers a unique perspective within the realm of medical imaging technologies. Unlike X-ray, CT, or MRI, which primarily visualize anatomy (form), PET visualizes metabolic processes (function). Modern scanners almost always combine PET with CT in a single hybrid machine (PET-CT). This powerful fusion overlays the functional data from the PET scan onto the detailed anatomical map provided by the CT scan.
The Science Behind the Image (Technical Principles)
The PET-CT process is a two-part system that provides a comprehensive diagnostic image.
- PET Component (Function):
- A patient is injected with a small amount of a radioactive tracer. The most common tracer is Fluorodeoxyglucose (FDG), a form of glucose tagged with a positron-emitting radioisotope (PMC, PubMed Central).
- Cells with high metabolic activity, such as cancer cells, rapidly growing tumors, or inflamed tissues, consume more glucose. Consequently, the FDG tracer accumulates in these “hot spots.”
- The radioactive tag on the FDG decays by emitting positrons. When a positron collides with a nearby electron in the body, they annihilate each other, producing two gamma rays that travel in opposite directions.
- A ring of detectors in the PET scanner registers these pairs of gamma rays. By analyzing the timing and location of these detections, a computer can map the areas of high metabolic activity.
- CT Component (Form): A standard CT scan is performed in the same session, providing a high-resolution anatomical image of the body’s structures.
- Image Fusion: The computer then fuses the two sets of images, overlaying the color-coded PET data (showing metabolic hot spots) onto the grayscale CT anatomical image. This allows clinicians to see exactly where the abnormal metabolic activity is occurring (RadiologyInfo.org).
Primary Clinical Applications
PET-CT is a cornerstone of modern oncology and has important uses in cardiology and neurology.
- Oncology: Essential for diagnosing cancer, staging (determining if and where it has spread), and monitoring the effectiveness of treatments like chemotherapy and radiation. It can often detect metabolic changes in tumors before they change in size on a CT or MRI.
- Cardiology: Used to assess the health of heart muscle, particularly after a heart attack, by differentiating between dead tissue and viable (hibernating) tissue that could benefit from intervention.
- Neurology: Helps in the diagnosis of dementia, including Alzheimer’s disease, by identifying patterns of decreased brain metabolism. It can also be used to locate the origin of seizures in the brain for surgical planning.
Head-to-Head: A Practical Comparison of Imaging Modalities
Quick Comparison Table
| Feature | X-ray | CT (Computed Tomography) | MRI (Magnetic Resonance Imaging) | PET-CT (Positron Emission Tomography) |
| Core Principle | X-ray Attenuation | Rotational X-ray Attenuation | Nuclear Magnetic Resonance | Radiotracer Metabolism + X-ray |
| Best For | Bones, Lungs, Dental | Trauma, Tumors, Blood Clots, Bones | Soft Tissues (Brain, Joints, Spine) | Functional/Metabolic Activity (Cancer) |
| Scan Time | < 1 minute | < 5-10 minutes | 30-60+ minutes | 1.5-2 hours (including uptake time) |
| Radiation Used | Yes (low dose) | Yes (higher dose) | No | Yes (from tracer and CT) |
Safety and Cost Analysis
Choosing the right medical imaging technologies involves a careful balance of diagnostic need, patient safety, and economic considerations. Each modality has a distinct profile in these areas.
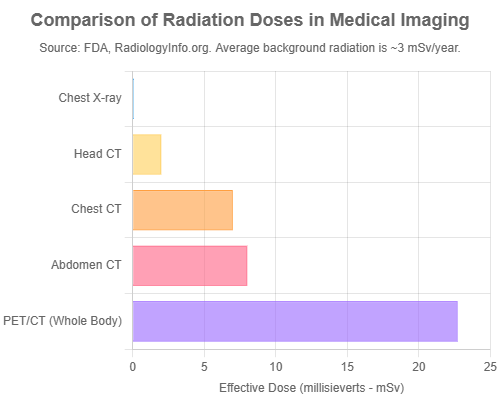
Radiation Exposure
A primary concern with X-ray and CT, both widely used medical imaging technologies, is the use of ionizing radiation, which has enough energy to potentially damage DNA and carries a small, cumulative lifetime risk of inducing cancer (U.S. FDA). This risk is managed by the ALARA (As Low As Reasonably Achievable) principle, where clinicians use the minimum radiation dose required to obtain a diagnostic-quality image.
To put doses into perspective:
- A standard chest X-ray delivers a dose of about 0.1 millisieverts (mSv), which is equivalent to about 10 days of natural background radiation.
- A CT scan of the chest delivers a much higher dose, around 7 mSv, equivalent to about 2 years of background radiation (RadiologyInfo.org).
- A whole-body PET/CT scan can have a combined dose of up to 25 mSv, with contributions from both the radiotracer and the CT component.
Crucially, MRI does not use ionizing radiation, making it a safer option for pediatric patients and individuals requiring frequent follow-up scans, provided it is clinically appropriate for the diagnostic question.
MRI Safety and Other Considerations
The main safety concern with MRI, one of the key medical imaging technologies, is its powerful magnetic field. Patients with certain metallic implants, such as older pacemakers, cochlear implants, or metal fragments in their eyes, cannot undergo an MRI. The loud, banging noise produced by the vibrating gradient coils is another factor, requiring patients to wear ear protection. Additionally, contrast agents used in both CT (iodine-based) and MRI (gadolinium-based) carry a small risk of allergic reaction or, in rare cases, can affect patients with poor kidney function.
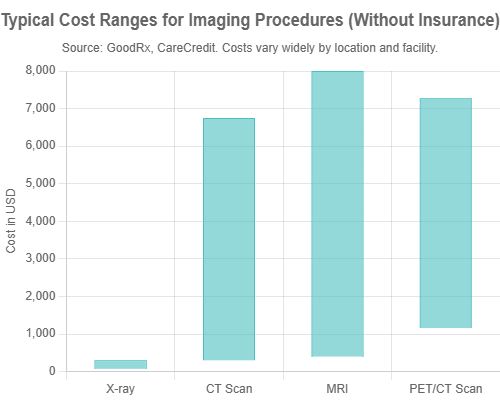
Cost Considerations
The cost of imaging procedures varies significantly, driven by equipment complexity, scan duration, and the need for specialized personnel or materials like radiotracers.
- X-ray: The most affordable, with costs typically ranging from $74 to $300 (GoodRx).
- CT Scan: More expensive than X-ray, with average costs ranging from $300 to over $6,000 depending on the body part and facility (CareCredit).
- MRI: Generally more expensive than CT due to longer scan times and more complex equipment.
- PET-CT: The most expensive modality, with costs often starting from $1,159 and reaching over $7,000, largely due to the high cost of producing and handling the short-lived radiotracers (CareCredit).
The Future of Medical Imaging: What’s Next?
The field of medical imaging is in a constant state of evolution, driven by technological innovation and the integration of artificial intelligence. The next decade promises to make imaging faster, safer, and more insightful than ever before.
Artificial Intelligence (AI) Integration
AI is poised to revolutionize radiology from the ground up. Its impact is being felt in two primary areas:
- Image Analysis and Diagnosis: Deep learning algorithms are being trained on vast datasets of medical images to detect subtle abnormalities—such as early-stage lung nodules or signs of stroke—with a speed and accuracy that can augment, and sometimes exceed, human capabilities (PMC, PubMed Central).
- Workflow Optimization: AI is streamlining the entire imaging process. It can help automate scan protocols for consistency, reduce image noise in low-dose scans (allowing for safer imaging), and triage cases by automatically flagging critical findings for immediate review by a radiologist (The Doctors Company).
Emerging Technologies
Beyond AI, fundamental hardware advancements are pushing the boundaries of what’s possible.
- Photon-Counting CT (PCCT): Hailed as the next major leap in CT technology, PCCT uses a new type of detector that directly counts individual X-ray photons and measures their energy levels. This results in significantly higher spatial resolution, reduced image noise, lower radiation doses, and the ability to better differentiate between different types of tissue and contrast materials (RadioGraphics).
- Whole-Body MRI: This technique is gaining traction as a radiation-free screening tool for detecting early-stage cancers in high-risk individuals, such as those with genetic predispositions (e.g., Li-Fraumeni syndrome). It offers a comprehensive, one-stop-shop assessment of the entire body (AJR).
- Hybrid Imaging Advances (PET/MRI): The development of PET/MRI scanners combines the metabolic insights of PET with the superior soft-tissue contrast and radiation-free nature of MRI. This is particularly promising for applications in neurology, pediatric oncology, and the evaluation of soft-tissue tumors where anatomical detail is paramount (PMC, PubMed Central).
Common Questions (FAQs)
Q1: Is a CT scan just a more powerful X-ray?
A: In a way, yes, but with a crucial difference. While both use X-rays, a standard X-ray creates a single, flat 2D image. A CT scan takes hundreds of X-ray images from multiple angles as it rotates around you and uses a computer to reconstruct them into detailed 3D cross-sectional “slices.” This provides far more depth and information abo
Q2: Why are MRIs so loud and take so long?
A: The loud banging and knocking sounds come from the rapid switching of the gradient coils. These coils create vibrations as they adjust the magnetic field to pinpoint the location of signals, and this vibration is what you hear. The long scan time is because MRI is not a single snapshot; it requires running multiple pulse sequences to capture images with different contrasts and from various angles to build a complete, detailed picture of the soft tissues.
Q3: Will I be radioactive after a PET scan?
A: Yes, you will be temporarily radioactive for a few hours after the injection of the radiotracer. The radioactive material is specifically chosen for its short half-life, meaning it decays quickly and is naturally flushed from your body through urine. As a precaution, you will be advised to avoid close, prolonged contact with pregnant women and young children for a short period (usually 6-12 hours) after the scan.
Q4: Why might I need an injection of “dye” (contrast agent)?
A: Contrast agents, often called “dyes,” are used in both CT and MRI to enhance the visibility of certain tissues or structures. For CT, an iodine-based agent helps highlight blood vessels, tumors, and organs. For MRI, a gadolinium-based agent serves a similar purpose. By making these areas stand out more clearly from the surrounding tissue, the contrast agent provides the radiologist with a more detailed and accurate view to make a confident diagnosis.
Conclusion: A Clearer Picture of Health
Medical imaging technologies are a diverse and powerful toolkit, each offering a unique window into the human body. From the foundational bone and lung assessments of X-ray to the detailed 3D anatomy of CT, the unparalleled soft-tissue clarity of MRI, and the functional metabolic insights of PET-CT, these tools are fundamental to modern healthcare. The choice of modality is a complex clinical decision, carefully balancing diagnostic necessity against critical factors like radiation safety, cost, and patient comfort.
The field of medical imaging technologies is advancing at a breathtaking pace. The integration of artificial intelligence and the development of next-generation hardware like photon-counting CT and PET/MRI are set to make imaging faster, safer, and more precise than ever. From Wilhelm Röntgen’s first shadowy image of a hand to today’s AI-enhanced 3D reconstructions, the journey of medical imaging is a remarkable testament to human ingenuity in the enduring quest to understand and heal the body.
What are your thoughts on the future of medical imaging? Do you have experience with these technologies as a professional or patient? Share your insights in the comments below! For more deep dives into the world of medical technology, subscribe to the MedTech Insighter newsletter.