Introduction
In the high-stakes environment of critical cardiac care, where every second and every heartbeat counts, mechanical circulatory support devices are true lifesavers. Among them, one device has remained a cornerstone for decades, a familiar presence in intensive care units and cardiac catheterization labs worldwide: the Intra-Aortic Balloon Pump (IABP).
The IABP machine is a fundamental tool for supporting the failing heart, but its true value lies in understanding its precise mechanics, appropriate application, and economic impact in an evolving healthcare landscape. While newer, more powerful devices have emerged, the IABP’s simplicity, cost-effectiveness, and extensive clinical familiarity ensure its continued relevance.
This comprehensive guide is tailored for a wide medical audience—ranging from students and nurses learning the basics to cardiologists, critical care physicians, biomedical engineers, and hospital procurement teams. It explains how the IABP machine works through the principle of counterpulsation, outlines its main clinical indications and contraindications, details its core components, and provides a clear cost and market outlook for 2025.
The Principle of Counterpulsation: How an IABP Machine Supports the Heart
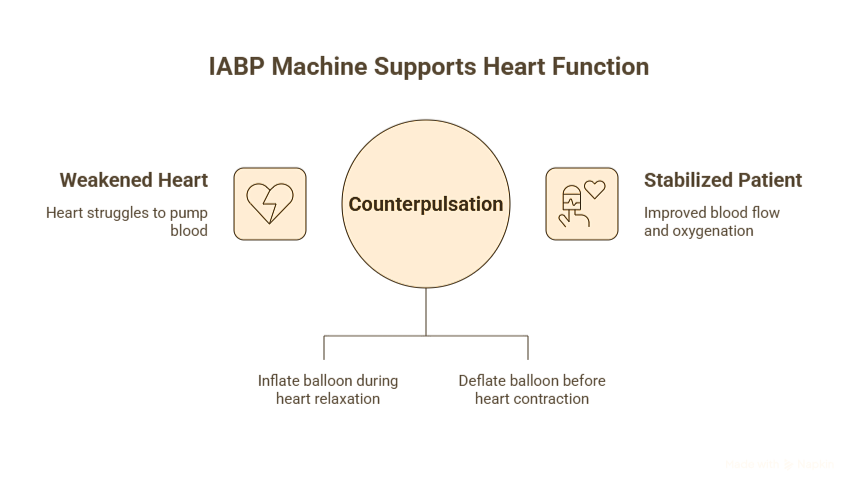
The scientific core of the IABP machine lies in a simple yet profound concept: counterpulsation. At its heart, the device works by performing the opposite action of the heart, in perfect synchrony with the cardiac cycle. It inflates when the heart rests and deflates when the heart pumps. This rhythmic opposition generates powerful hemodynamic benefits that can stabilize a critically ill patient.
The Two-Step Process: A Symphony of Inflation and Deflation
The therapeutic effect of the IABP is delivered through a precise, two-step process orchestrated by the machine’s console, which is timed to the patient’s own heart rhythm.
1. Diastolic Inflation: Feeding the Heart and the Body
At the onset of diastole (the period when the heart relaxes and fills with blood), the long, sausage-shaped balloon, positioned in the descending aorta, rapidly inflates with helium. This inflation has two immediate, critical effects:
- Increased Coronary Perfusion: When the IABP machine inflates during diastole, the balloon displaces 30–50 cc of blood, raising pressure in the aortic root (diastolic augmentation). This forces more oxygen-rich blood back into the coronary arteries—the vessels that nourish the heart muscle. In effect, it “force-feeds” the myocardium with oxygen and nutrients, which is especially critical during ischemic events such as a heart attack.
- Increased Systemic Perfusion: This same increase in diastolic pressure helps improve blood flow to vital organs throughout the body, a crucial benefit for patients in cardiogenic shock who are often severely hypotensive.
2. Systolic Deflation: Lightening the Heart’s Load
Just moments before the left ventricle contracts to eject blood into the aorta (systole), the balloon rapidly deflates. This sudden deflation creates a transient vacuum or area of lower pressure in the aorta. The effect is profound:
- Decreased Afterload: Afterload is the resistance the heart must overcome to eject blood. When the IABP machine deflates just before systole, it creates a low-pressure “sink” in the aorta, dramatically reducing this resistance. As a result, the left ventricle pumps more efficiently with less effort, lowering oxygen demand and easing the workload on a weakened heart muscle (BJA Education, 2009).
Technical Deep Dive & Visual Aid: The IABP Waveform
The combined effects of inflation and deflation are best seen on an arterial pressure waveform. The IABP machine console continuously monitors the patient’s blood pressure and displays a distinctive waveform that confirms proper function. Modern systems also use advanced algorithms—often triggered by the ECG R-wave or pressure waveform—to optimize timing, ensuring accurate counterpulsation even in patients with severe arrhythmias (Teleflex).
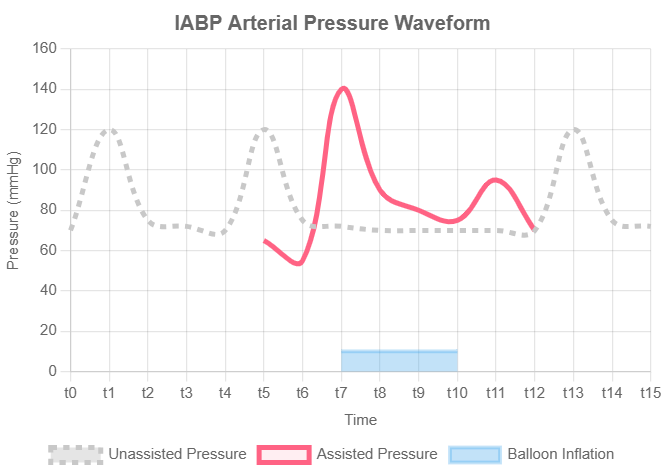
Figure 1: Hemodynamic Effects of IABP Counterpulsation. This chart illustrates how the IABP inflates during diastole to augment pressure (increasing coronary perfusion) and deflates before systole to reduce afterload (decreasing the heart’s workload).
Clinical Applications: When to Use an IABP Machine
The IABP is not a cure but a powerful supportive tool. It is best understood as a “bridge”—a temporary measure to stabilize a patient, allow for myocardial recovery, or enable a more definitive treatment. Its use is indicated in several critical clinical scenarios where the heart’s pumping function is severely compromised.
Based on guidelines and clinical practice reviews, the primary indications include:
- Cardiogenic Shock: This is the main condition where an IABP machine is used. In cardiogenic shock—often caused by a major heart attack or severe heart failure—the heart is too weak to pump enough blood for the body. The IABP machine helps by improving blood flow to vital organs, giving doctors time to treat the underlying problem (Cleveland Clinic).
- High-Risk Angioplasty (PCI): In patients with severe blockages or a weak heart, stent procedures can be risky. The IABP machine is sometimes used as a safety backup to keep blood flow stable and protect the heart during angioplasty or stent placement (LITFL).
- Support for Cardiac Surgery: The IABP machine can be used before heart bypass surgery to stabilize high-risk patients, or after surgery if the heart is too weak to work properly without the heart-lung machine (AATS).
- Complications After a Heart Attack: Sometimes a severe heart attack can damage the heart’s walls or valves, causing life-threatening problems. In these cases, the IABP machine helps reduce strain on the heart and keeps blood flowing until the patient can have emergency surgery (StatPearls).
- Bridge to Definitive Therapy: In patients with severe heart failure, the IABP machine can act as a temporary support system. It keeps them stable until they receive a permanent treatment, such as a heart transplant or a long-term heart pump (Left Ventricular Assist Device)(LVAD).

When to Avoid IABP: Key Contraindications
While the IABP is a powerful tool, its mechanics can be harmful in certain conditions. Understanding the contraindications is as critical as knowing the indications. The decision to place an IABP requires careful patient assessment to avoid causing iatrogenic harm.
The absolute contraindications, where IABP use is considered dangerous, include:
- Moderate to Severe Aortic Regurgitation: In this condition, the aortic valve does not close properly and leaks blood backward. If the balloon inflates, it pushes even more blood the wrong way, overloading the weak heart and worsening heart failure, which can lead to fluid in the lungs (Deranged Physiology).
- Aortic Dissection: This is a tear in the wall of the aorta. Using the balloon here can make the tear worse, block blood flow to vital organs, or even cause the aorta to rupture, which is life-threatening (OpenAnesthesia).
- Severe Peripheral Artery Disease (PVD): In this condition, the arteries in the legs are already narrowed or blocked. Inserting the balloon catheter through these vessels can damage them further, possibly cutting off blood flow to the leg.
- Uncontrolled Sepsis and Bleeding Disorders: In patients with severe infection (sepsis), inserting a large catheter can worsen the infection and spread it through the bloodstream. In those with bleeding problems, the insertion site can lead to dangerous, uncontrolled bleeding (LITFL CCC).
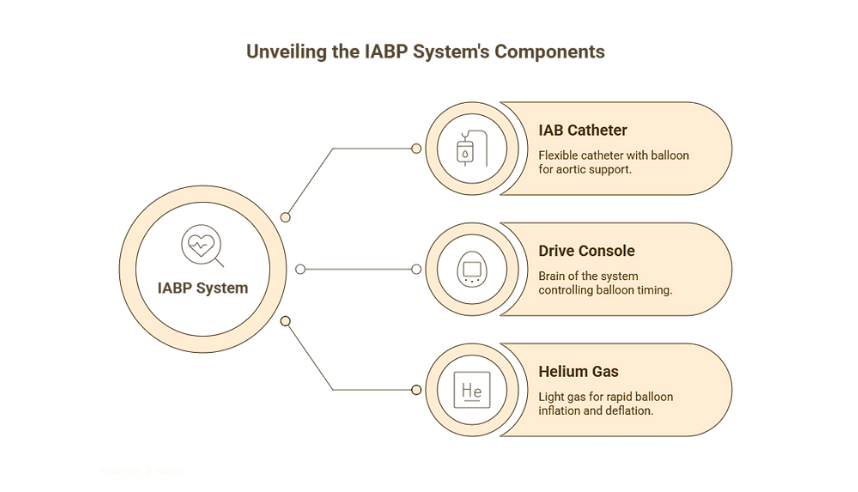
Anatomy of the System: The Parts of an IABP Machine
The IABP system, though complex in its function, consists of three primary components. Understanding each part is essential for clinicians managing the therapy and for biomedical engineers responsible for its maintenance.
Anatomical diagram of an Intra-Aortic Balloon Pump system, showing the catheter with its balloon, helium and blood lumens, and its connection to the external console and helium tank
| Component | Core Function & Key Features | Notes for Clinical & Technical Staff |
|---|---|---|
| The IAB Catheter | A long, flexible catheter with a sausage-shaped balloon at the tip. It has one channel for inserting a guidewire and monitoring blood pressure, and another sealed channel for moving gas in and out of the balloon. | Sizing: Catheters come in various sizes (e.g., 7.5 Fr), with balloon volumes (30, 40, or 50 cc) selected according to the patient’s height. The goal is for the balloon to fill about 80–90% of the aorta without blocking important arteries.(LITFL). Technology: Some modern catheters use fiber-optic sensors to detect pressure changes more quickly and accurately, helping the balloon inflate and deflate at the right time. |
| The Drive Console | This is the “brain” of the system. It contains the pump that moves helium in and out of the balloon, the computer that controls timing, and a large display screen for the user. | Features: Modern consoles, such as those from Teleflex (AC3 Optimus™) and Getinge (Cardiosave), have high-definition touchscreens, smart algorithms that automatically adjust timing during irregular heartbeats, and portable designs to safely move patients between hospital departments. |
| Helium Gas | The specific gas used to inflate and deflate the balloon. It is supplied from a small, dedicated tank housed within or attached to the console. | Why Helium? Helium is very light, which lets the balloon inflate and deflate quickly in sync with the heartbeat, even at fast rates. It’s also safe—because helium doesn’t react with the body and dissolves easily in blood, so if the balloon ever ruptures, the gas is absorbed without causing serious harm (Deranged Physiology). |
Anatomy of IABP System
The 2025 IABP Machine Price & Market Landscape
For hospital administrators, procurement teams, and health economists, understanding the financial and market dynamics of the IABP machine is crucial. In an era of value-based care, the IABP’s position is defined as much by its cost-effectiveness as its clinical efficacy.
Understanding the Cost of IABP Therapy
The cost of IABP therapy can be broken down into three main components: the initial capital investment, the per-procedure disposable costs, and the overall impact on the cost of hospitalization.
- Capital Equipment Cost (Console): The console is a one-time purchase for hospitals. Prices depend on the brand, model, and features like portability or advanced software. To save money, many hospitals choose refurbished consoles from trusted vendors.
- Per-Procedure Cost (Disposable Catheter): Each IABP treatment requires a single-use catheter, costing about $800–$1,200 in 2025. In comparison, advanced devices like the Impella can cost around $20,000 each (A Value-Based Analysis of Hemodynamic Support). This huge price difference is a key reason why the IABP is still widely used, especially in hospitals with limited resources.
- Impact on Total Hospitalization Cost: Although the IABP device itself is affordable, patients who need it are usually very sick and require longer ICU care. This adds to hospital expenses. A 2020 study found that IABP therapy increased total hospital costs by about $14,364 compared to standard medical treatment, mainly due to extended ICU stays and intensive monitoring (Millet et al., 2020).
Market Snapshot: Key Players and Innovations
Global Market Overview: The IABP market is well established but still growing. In 2024, it was worth over $430 million and is expected to reach about $445 million in 2025, with steady growth of 3–4% per year. This rise is driven mainly by increasing heart disease cases and an aging population (Global Growth Insights, 2025).
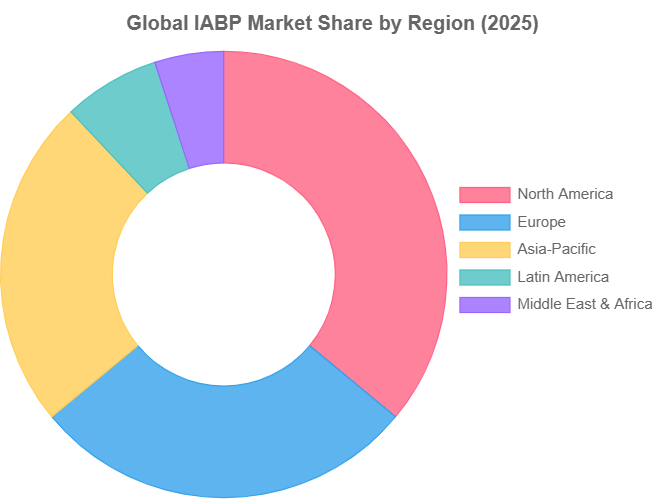
Figure 2: Global IABP Market Share by Region (2025). North America remains the dominant market, but the Asia-Pacific region is experiencing rapid growth. Data sourced from Global Growth Insights.
The market is dominated by a few key MedTech giants:
- Teleflex (owning Arrow): A major player known for its AC3 Optimus™ and transport-ready AC3 Range™ IABP systems.
- Getinge (owning Maquet): A global leader with its Cardiosave line of IABP consoles, which are widely used in European and US hospitals.
- Abiomed: While primarily known for its Impella devices, Abiomed often positions the IABP as a primary stabilizer in its hybrid care protocols.
Key innovations shaping the market in 2025 and beyond include:
- Enhanced Portability: There is a strong trend towards smaller, lighter, and more rugged consoles designed for seamless patient transport, whether by ground ambulance or air.
- Smarter Algorithms: Modern systems now use AI and advanced software to improve balloon timing, even in patients with irregular heartbeats. This reduces the need for doctors to make frequent manual adjustments.
- EMR and Data Integration: New consoles can connect directly with hospital electronic medical record (EMR) systems, making it easier to manage patient data, enable remote monitoring, and support clinical research.
- Miniaturization of Catheters: Ongoing R&D focuses on developing smaller, less invasive catheters to reduce the risk of vascular complications, which remain the Achilles’ heel of the therapy.
Weighing the Options: Advantages and Limitations of IABP
No medical device is without its trade-offs. A balanced understanding of the IABP’s pros and cons is essential for sound clinical judgment.
Advantages
- Cost-Effective: As detailed above, the per-procedure device cost is dramatically lower than other temporary mechanical circulatory support options like pVADs (Impella) or Extracorporeal Membrane Oxygenation (ECMO).
- Widely Available & Familiar: The IABP machine is found in almost every cardiac center worldwide. Doctors, surgeons, and critical care staff are highly experienced in using and managing it.
- Relatively Simple and Quick Insertion: A trained doctor can place the IABP catheter through the skin at the bedside or in the cath lab within a short time, making it very useful in emergencies.
- Proven Hemodynamic Benefits: For decades, it has been proven to reliably achieve its primary goals: increasing coronary perfusion and reducing left ventricular workload.
Limitations & Potential Complications
- Patient Immobility: Patients must stay on strict bed rest with limited movement to keep the catheter safe. This lack of mobility can lead to other health problems.
- Vascular Complications: The biggest drawback is the large catheter, which can reduce blood flow to the leg, cause bleeding, or damage the blood vessel. Careful monitoring of leg pulses and circulation is essential.
- Dependence on Heart Rhythm: The IABP is only a support device, not a full heart pump. It needs the patient’s own heartbeat to work, so it cannot help during cardiac arrest or very severe irregular rhythms.
- Thrombocytopenia: A mild drop in platelet count can happen because of the balloon’s contact with blood, but it is usually not serious.
Frequently Asked Questions (FAQs)
Q1: How does an IABP machine differ from an Impella device?
The fundamental difference is in the mechanism of support. An IABP provides indirect support through counterpulsation; it assists the heart’s own pumping action. In contrast, an Impella is a miniaturized axial flow pump that provides direct support. It actively pulls blood from the left ventricle and ejects it into the aorta, directly unloading the ventricle and propelling blood forward. Impella provides significantly more hemodynamic support (higher cardiac output) but is far more expensive and can be more complex to manage (AHA Journals).
Q2: Is IABP therapy a permanent solution?
No. The IABP machine is strictly a temporary support measure. It is typically used for a period of hours to a few days. It serves as a bridge—a bridge to myocardial recovery, a bridge to a definitive surgical procedure (like CABG or valve replacement), or a bridge to a long-term support device (like an LVAD) or heart transplantation (Cleveland Clinic).
Q3: What happens if the IABP balloon ruptures?
This is a rare but serious complication. The choice of helium as the inflation gas is a key safety feature. Because helium is inert and has very low solubility in blood, if a rupture occurs, the small gas bubbles are typically absorbed by the blood without causing a clinically significant gas embolism, which would be a major risk if air were used. The drive console is also designed to detect a leak or rupture instantly, stopping the pump and sounding a critical alarm, allowing for immediate removal of the device (LITFL).
Conclusion: The Enduring Role of the IABP Machine in 2025
In modern cardiac care, the IABP machine remains a vital and cost-effective support tool. While it cannot match the power of newer devices, its reliability, simplicity, and lower cost keep it important worldwide. By understanding counterpulsation, knowing when to use it, and recognizing its value, healthcare professionals can continue to rely on this proven technology to stabilize critically ill patients and improve outcomes.
The landscape of mechanical circulatory support is constantly evolving. What are your experiences with the latest IABP models or competing technologies like Impella and ECMO? How has your institution’s approach to hemodynamic support changed in recent years? Share your insights and questions in the comments below to foster a community of learning at MedTech Insighter!
“If you’re interested in how technology is shaping the future of healthcare, you may also like our article on AI in breast cancer detection, which highlights how artificial intelligence is transforming diagnosis.”