Introduction: Beyond Conventional Breathing Support
Imagine a patient with severe Acute Respiratory Distress Syndrome (ARDS). Their lungs are stiff, inflamed, and failing. With every breath delivered by a conventional mechanical ventilator, the delicate air sacs (alveoli) are forced open and then collapse, causing further injury. Despite the clinical team’s best efforts, the patient’s oxygen levels continue to fall. What is the next step when standard life support is not enough? Medical professionals attending to a critically ill patient in an intensive care unit, a common setting for advanced ventilation strategies.
The High-Frequency Oscillation Ventilator (HFOV) offers a radically different method of lung support, especially for patients with severe respiratory failure. Rather than delivering large, forceful breaths, HFOV uses constant gentle pressure and rapid, small-volume oscillations to maintain lung inflation and improve gas exchange—minimizing further injury.
This comprehensive guide explains how the High-Frequency Oscillation Ventilator works, reviews clinical evidence, and outlines when and how it can be a life-saving option. Designed for clinicians, biomedical engineers, and students, it covers HFOV’s core mechanics, clinical uses, pros and cons, and answers to key questions.
Table of Contents
How HFOV Works: A Paradigm Shift in Ventilation
To appreciate HFOV, one must move past the traditional concept of breathing. It operates on principles that seem counterintuitive at first but are grounded in sophisticated respiratory physiology and fluid dynamics.
The Fundamental Principle: “Open Lungs, Quiet Lungs”
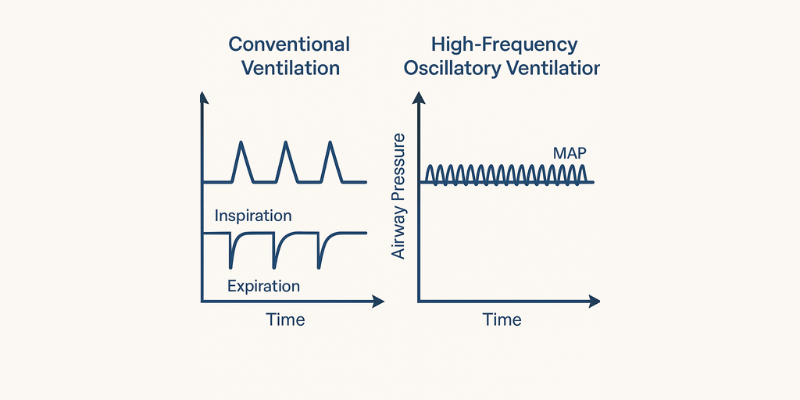
The core philosophy of HFOV is to prevent ventilator-induced lung injury (VILI). Conventional ventilation (CV) involves a cyclical “inflate-deflate” process. In a stiff, sick lung, this can lead to two types of damage:
- Volutrauma: Overstretching of alveoli from excessive volume or pressure.
- Atelectrauma: Repetitive opening and closing of unstable alveoli, causing shear stress and inflammation.
The High-Frequency Oscillation Ventilator (HFOV) maintains a constant Mean Airway Pressure (MAP) to open and stabilize collapsed lung areas, creating a consistent lung volume. Around this pressure, HFOV delivers rapid, tiny breaths—often smaller than anatomical dead space—reducing the risk of ventilator-induced lung injury. This “open lung, quiet lung” approach, as described in a review on the topic, minimizes cyclic stretch and helps preserve end-expiratory lung volume.
The Engine of Oscillation: How HFOV Generates Flow
The “magic”; of HFOV lies in its mechanism for generating rapid, bi-directional airflow. Unlike conventional ventilators where exhalation is passive, HFOV actively pushes gas in and pulls it out.
The most common technology is the piston/diaphragm oscillator. Devices like the Sensormedics 3100B use an electromagnetically controlled diaphragm that vibrates at high frequencies. This vibration acts like a loudspeaker, creating pressure waves that travel down the airway. This mechanism generates a near-perfect sine wave of pressure, ensuring both an active inspiratory and an active expiratory phase. Other hybrid systems, such as those found in ventilators like the Dräger VN500, use different technologies like flow interrupters or opposing gas flows to achieve a similar oscillatory effect, sometimes allowing for more varied waveforms.
Gas Exchange Without Large Breaths: The Science of Diffusion and Mixing
If the tidal volumes are smaller than the dead space, how does oxygen get in and carbon dioxide get out? The answer lies in several complex gas transport mechanisms that are enhanced by the high-frequency oscillations:
- Augmented (Taylor) Dispersion: The rapid, turbulent flow creates a unique profile where fresh gas jets down the center of the airways, while expired gas moves out along the airway walls. This dramatically enhances gas mixing.
- Pendelluft: In an unevenly diseased lung, some regions fill and empty faster than others. The oscillations cause gas to shuttle between adjacent lung units with different mechanical properties, improving ventilation in slower-filling alveoli.
- Asymmetric Velocity Profiles: The velocity profile of the inspiratory wavefront is blunter than the expiratory wavefront, resulting in a net forward movement of gas deep into the lungs over many cycles.
- Cardiogenic Mixing: The physical beating of the heart against the lungs provides additional, low-frequency mixing of gases at the alveolar level.
- Direct Alveolar Ventilation: The alveoli closest to the main airways are still ventilated directly by the small tidal volumes.
These mechanisms work in concert to achieve effective gas exchange without requiring large, potentially damaging breaths. This complex interplay is detailed in technical guides on HFOV theory.
Controlling the Oscillator: Key Parameters and Their Effects
A key advantage of HFOV is the ability to independently manage oxygenation and ventilation. This is done by adjusting four primary parameters:
- Mean Airway Pressure (MAP): This is the primary control for oxygenation. By setting the constant distending pressure, the MAP recruits alveoli and optimizes the lung volume for gas exchange. It is analogous to PEEP in conventional ventilation, but it represents the average pressure throughout the entire respiratory cycle.
- Amplitude (ΔP) or Power: This determines the force of the oscillation, or the size of the pressure swing around the MAP. It is the primary control for ventilation (CO₂ removal). A higher amplitude displaces more gas with each oscillation, leading to greater CO₂ clearance. This is visually observed as the “chest wiggle” on the patient.
- Frequency (Hertz): This is the speed of the oscillations (1 Hz = 60 breaths/min). In most HFOV systems, there is an inverse relationship between frequency and ventilation. Decreasing the frequency allows more time for each oscillation, which increases the effective tidal volume and thus improves CO₂ removal. This is a critical and often misunderstood concept, as it is the opposite of conventional ventilation.
- Inspiratory Time % (I:E Ratio): This is typically fixed at 33% (an I:E ratio of 1:2) to provide a longer expiratory phase. This helps prevent air trapping, especially at high frequencies.
Clinical Application: Navigating the Evidence and Indications
While the theory behind HFOV is compelling, its clinical application has been a subject of intense debate, particularly in adults. Understanding the evidence is crucial for appropriate patient selection.
Who is a Candidate for HFOV? Primary Indications
HFOV is almost exclusively used as a rescue therapy when conventional lung-protective strategies have failed. It is not a first-line treatment.
- Adults: The primary indication is severe ARDS with refractory hypoxemia (e.g., a PaO₂/FiO₂ ratio below 100-150) despite optimized conventional ventilation, including high PEEP and potentially prone positioning.
- Neonates & Pediatrics: HFOV has a more established and broader role in this population. According to clinical reviews, common indications include:
- Persistent Pulmonary Hypertension of the Newborn (PPHN): Where maintaining lung volume can improve pulmonary vascular resistance.
- Meconium Aspiration Syndrome (MAS): HFOV can help recruit lungs affected by surfactant inactivation and inflammation.
- Severe Respiratory Distress Syndrome (RDS).
- Air Leak Syndromes: Conditions like pulmonary interstitial emphysema or bronchopleural fistulas, where the low tidal volumes of HFOV can reduce air leakage and allow tissues to heal.
- Persistent Pulmonary Hypertension of the Newborn (PPHN): Where maintaining lung volume can improve pulmonary vascular resistance.

Diagnosing and managing severe ARDS often requires the integration of advanced ventilator strategies like HFOV and modern diagnostic tools such as medical imaging technologies to monitor lung pathology and treatment response.
The Great Debate: Clinical Evidence on High-Frequency Oscillation Ventilator (HFOV)
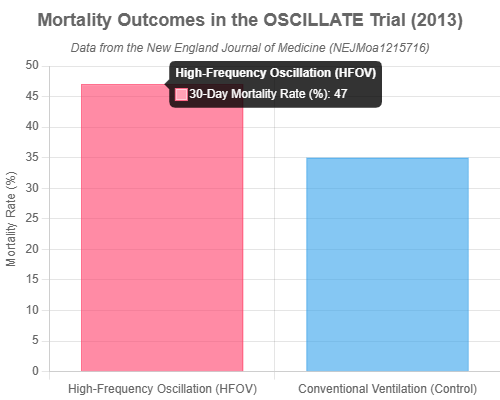
The clinical use of the High-Frequency Oscillation Ventilator (HFOV) in adults faced setbacks after two major randomized controlled trials in 2013—OSCAR and OSCILLATE—found no significant benefit over conventional ventilation in moderate-to-severe ARDS cases. These findings led to reduced adoption of HFOV in adult critical care despite its theoretical advantages.
- The OSCAR trial found no difference in mortality.
- The OSCILLATE trial was stopped early due to increased mortality in the HFOV group (47% vs. 35% in the conventional ventilation group).
Despite the initial decline in adult use of the High-Frequency Oscillation Ventilator (HFOV) following the OSCAR and OSCILLATE trials, later reviews highlighted important limitations in study design and patient selection. For example, the OSCILLATE trial’s aggressive recruitment strategy may have caused hemodynamic instability. This has led to a consensus that HFOV is not suitable for mild or moderate ARDS, but may still offer benefits in severe ARDS cases (PaO₂/FiO₂ < 100) where conventional therapies fail. These findings suggest that the problem lies more in application than in the technology itself.
HFOV vs. Conventional Ventilation: A Head-to-Head Comparison
| Feature | High-Frequency Oscillation (HFOV) | Conventional Ventilation (CV) |
|---|---|---|
| Primary Goal | Lung recruitment and protection | Maintain minute ventilation |
| Tidal Volume | Very low (often < dead space) | Low, but > dead space (4-6 mL/kg) |
| Respiratory Rate | Very high (3-15 Hz / 180-900 bpm) | Physiological (12-35 bpm) |
| Airway Pressure | High, constant mean pressure | Cyclical (peak and PEEP) |
| Mechanism | Active inspiration and expiration | Active inspiration, passive expiration |
| Primary Use Case | Rescue for severe ARDS, neonatal failure | First-line for most respiratory failure |
The Strengths and Limitations of High-Frequency Oscillation Ventilator (HFOV)
The Strengths: Why Choose HFOV?
- Lung Protection: The High-Frequency Oscillation Ventilator (HFOV) reduces ventilator-induced lung injury (VILI) by minimizing pressure swings and maintaining continuous alveolar recruitment—especially effective in preventing atelectrauma.
- Improved Oxygenation: In severe cases of refractory hypoxemia, HFOV can reopen collapsed lung tissue and significantly boost oxygen levels when conventional ventilation fails.
- Air Leak Management: For conditions like pneumothorax or bronchopleural fistulas, HFOV’s low tidal volumes and stable pressure help minimize gas leakage and promote healing.
Limitations of High-Frequency Oscillation Ventilator (HFOV)
- Hemodynamic Instability: The constant high intrathoracic pressure from the High-Frequency Oscillation Ventilator (HFOV) can reduce cardiac output and cause hypotension, requiring close monitoring and fluid or vasopressor support.
- Barotrauma & Air Trapping: Improper use—especially with high MAP or in patients with obstructive airway disease—can lead to lung over-distension, air trapping, or pneumothorax.
- Need for Deep Sedation: HFOV typically requires deep sedation and neuromuscular blockade, increasing the risk of ICU-acquired weakness and prolonged hospitalization.
- Monitoring Difficulties: The machine’s vibrations and noise complicate traditional assessments like auscultation, and any disconnection (e.g., for suctioning) risks lung derecruitment.
- Steep Learning Curve: Effective HFOV management demands an experienced multidisciplinary team familiar with its unique physiology and risks.
Common Questions and Practical Answers (FAQ)
How do you separately manage oxygenation and CO₂ on HFOV?
his is a key advantage. Oxygenation is primarily controlled by adjusting the Mean Airway Pressure (MAP) to recruit lung volume and the FiO₂. CO₂ removal (ventilation) is primarily controlled by adjusting the Amplitude (ΔP) and, secondarily, by decreasing the Frequency.
Are there any absolute contraindications for HFOV?
Most sources state there are no absolute contraindications, but there are strong relative ones where the risk may outweigh the benefit. These include severe obstructive airway disease (e.g., asthma, severe COPD), unmanaged pneumothorax, and severe hemodynamic instability that is unresponsive to fluids and vasopressors. Caution is also advised in patients with intracranial hypertension, as high MAP can impede cerebral venous return.
How do you wean a patient from HFOV?
Weaning is a careful, gradual process. First, the FiO₂ is reduced to non-toxic levels (e.g., ≤0.40). Then, the MAP is slowly decreased in small steps (1-2 cmH₂O at a time), while closely monitoring oxygenation for signs of lung derecruitment. Once the patient is stable on minimal settings (e.g., MAP ≤16-17 cmH₂O, Amplitude low), they are typically transitioned back to a conventional ventilator for a period before considering extubation.
Conclusion: HFOV—A Specialized Tool for Critical Respiratory Failure
The High-Frequency Oscillation Ventilator (HFOV) is a complex yet powerful rescue therapy—not a first-line option. Its value lies in its unique lung-protective approach, making it especially effective for patients with severe respiratory failure when conventional ventilation fails.
While HFOV hasn’t consistently improved outcomes in adult ARDS populations, it remains a vital tool in neonatal and pediatric care. The key takeaway: successful use of HFOV depends on careful patient selection and expert clinical application. When used correctly, it can be life-saving in the most challenging cases.