Introduction: A New Symphony of Surgical Precision
For decades, surgeons have balanced precise tissue dissection with the need to control bleeding. Traditional tools like scalpels and electrocautery often involved trade-offs—thermal damage, slower procedures, or complex techniques. Enter the Harmonic Scalpel: a surgical innovation that uses high-frequency ultrasonic vibration to cut and coagulate simultaneously, offering precise, efficient, and low-thermal-damage performance.
The Harmonic Scalpel is not a future concept—it’s a present-day surgical breakthrough. Since its debut in the 1990s, it has redefined energy-based surgery with a unique ultrasonic mechanism. For surgeons, it means better outcomes and fewer complications. For biomedical engineers, it’s a benchmark in innovation. And for OR teams, mastering its use is key to safe, efficient procedures.
This deep dive will deconstruct the science behind the Harmonic Scalpel, analyze its evidence-based performance across key surgical specialties, benchmark it against conventional and advanced energy devices, and provide practical, actionable insights for every member of the surgical team.
Table of Contents

The Science of Sound: How the Harmonic Scalpel Works
The Core Principle: From Ultrasonic Vibration to Surgical Action
At its heart, the Harmonic Scalpel operates on a principle that is both elegant and powerful: the conversion of energy. The system takes electrical energy from a dedicated generator and, through a sophisticated transducer, transforms it into high-frequency mechanical motion. The active blade of the instrument vibrates longitudinally at an astonishing rate, typically 55,500 times per second (55.5 kHz), over a microscopic excursion of 50 to 100 micrometers. This rapid vibration is the engine of its surgical effect.
Unlike electrocautery, which uses high temperatures (150°C–400°C) by passing electrical current through tissue, the Harmonic Scalpel operates through controlled ultrasonic friction. Its vibrating blade generates heat at a much lower range (50°C–100°C), interacting with tissue at the molecular level. This denatures proteins by breaking hydrogen bonds—similar to whisking egg whites. This denaturation has a dual effect:
- Precise Cutting: The high-speed mechanical vibration cleanly and precisely separates tissue planes, allowing for delicate dissection.
- Reliable Coagulation: The Harmonic Scalpel denatures proteins to form a sticky coagulum. When combined with pressure from the instrument’s jaws (coaptation), this coagulum seals blood vessels effectively. Advanced models like the HARMONIC ACE®+7 Shears can reliably seal vessels up to 7 mm in diameter—highlighting their strong hemostatic capability. (PMC, The Harmonic Scalpel).
A key advantage of the Harmonic Scalpel is its minimal lateral thermal spread. Its low-temperature mechanism confines heat to the blade-tissue interface, greatly reducing collateral damage—crucial when operating near vital structures like nerves, vessels, or the bowel.
Anatomy of the System: A Guide for Engineers and OR Staff
Understanding the components of the Harmonic Scalpel system is fundamental for its correct assembly, use, and troubleshooting. The system is a synergistic assembly of three primary parts:
- The Generator: This is the “brain” and power source of the system. It’s a sophisticated electronic unit that produces the precise high-frequency electrical signal required to drive the handpiece. Modern generators often feature adaptive technology that can monitor tissue conditions and modulate energy output in real-time for optimal performance.
- The Handpiece (Transducer) is the electromechanical core of the Harmonic Scalpel. Inside, piezoelectric crystals—placed between metal cylinders—convert electrical signals from the generator into rapid, high-frequency vibrations by expanding and contracting. This conversion drives the scalpel’s cutting and coagulating action (World Laparoscopy Hospital).
- The Blade (End Effector): This is the single-use, patient-contact part of the Harmonic Scalpel. It includes a shaft and a specialized tip (e.g., shears, curved blades, hooks) suited for different procedures. The vibrating active blade cuts, while the inactive upper arm applies pressure to aid in coagulation.
Diagram: Harmonic Scalpel System Components
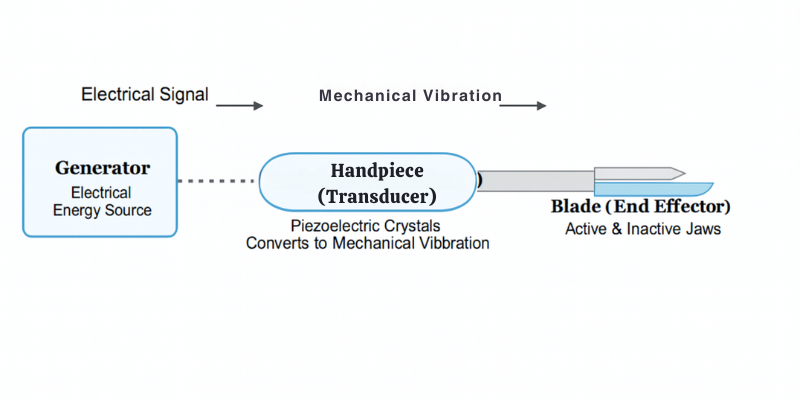
This diagram illustrates the energy conversion pathway: The Generator creates an electrical signal, which travels via a cable to the Handpiece. Inside the handpiece, piezoelectric crystals convert this into mechanical vibration, which is transmitted down the shaft to the Blade, where the surgical work is performed.
Clinical Performance: Where the Harmonic Scalpel Excels (Core Analysis)
The Evidence-Based Advantage: A Meta-Analysis Overview
The widespread adoption of the Harmonic Scalpel is backed by extensive clinical evidence. Over the past two decades, randomized controlled trials (RCTs), systematic reviews, and meta-analyses have consistently shown its advantages over traditional methods like cold scalpel dissection and electrocautery. Recent umbrella reviews further validate its effectiveness across multiple surgical specialties.
A landmark 2023 umbrella review in BMC Surgery, analyzing 24 systematic reviews and 83 RCTs, confirmed the clinical advantages of Harmonic Scalpel devices. Compared to conventional methods, Harmonic use showed statistically significant or consistent improvements in key patient outcomes (BMC Surgery, Umbrella Review 2023). The major performance benefits include:
- Reduced Operating Time: A consistently reported benefit, as cutting and coagulating with one tool eliminates frequent instrument changes. The umbrella review showed operating times were reduced by at least 25 minutes, with one meta-analysis on neck dissection noting a 29.3-minute average reduction (PMC, Neck Dissection Meta-Analysis)
- Decreased Intraoperative Blood Loss: The device’s effective sealing creates a drier surgical field. The 2023 umbrella review reported significant blood loss reductions in procedures such as cholecystectomy, colectomy, gastrectomy, mastectomy, and thyroidectomy.
- Improved Postoperative Recovery: Benefits include reduced pain, lower drainage volumes, and shorter hospital stays. In mastectomy cases, the review noted a significant decrease in length of stay.
- Lower Complication Rates: Reduced thermal damage and blood loss contribute to fewer complications. The umbrella review found consistent numerical improvements in overall complication rates across all evaluated meta-analyses.
It’s important to recognize the role of heterogeneity in surgical research. Variations in surgeon skill, patient populations, and techniques can affect study outcomes. For example, the neck dissection meta-analysis reported significant results but noted high statistical heterogeneity, requiring sensitivity analyses (PMC, Neck Dissection Meta-Analysis). Still, the overall trend from high-quality evidence strongly supports the clinical superiority of the Harmonic Scalpel over traditional methods.
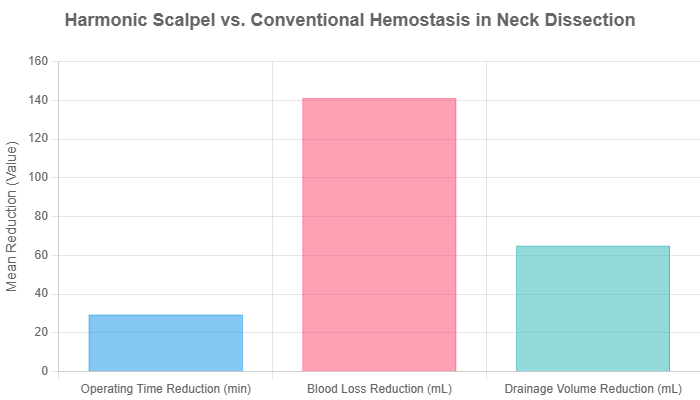
Chart: Mean Improvement in Surgical Outcomes for Neck Dissection using Harmonic Scalpel vs. Conventional Hemostasis. Data sourced from a meta-analysis of seven randomized controlled trials (Zhang et al., 2015). Note: The source study reported high statistical heterogeneity for these outcomes, which is common in surgical meta-analyses.
Spotlight on Surgical Specialties
The theoretical advantages of the Harmonic Scalpel translate into tangible benefits across a multitude of surgical disciplines. Its utility is most pronounced in procedures where precision and the preservation of delicate structures are paramount.
- Head and Neck Surgery (Thyroidectomy, Parotidectomy, Neck Dissection): This is one of the most impactful uses of the Harmonic Scalpel. Its minimal thermal spread helps protect vital nerves like the recurrent laryngeal (thyroidectomy) and facial nerve (parotidectomy), reducing risks of hoarseness and facial paralysis. In neck dissections, it efficiently controls small vessels, lowering blood loss and shortening operative time—as supported by meta-analysis data.
- Minimally Invasive Surgery (Laparoscopic & Robotic): In procedures like cholecystectomy and colectomy, the Harmonic Scalpel enhances efficiency by producing less surgical smoke, improving laparoscopic visibility. Its ability to cut and coagulate reduces the need for frequent instrument changes, streamlining workflow in tight operative spaces (EBME Clinical Engineering).
- Gynecologic and Oncologic Surgery: In procedures like hysterectomies and tumor resections, the Harmonic Scalpel enables precise dissection with reliable hemostasis—critical near major vessels and organs. It supports both oncologic and patient safety. In breast cancer surgery, studies show reduced drainage volume and lower rates of seroma formation (Indian Journal of Cancer).
- Other Expanding Fields: The device’s versatility has led to its widespread adoption in thoracic surgery (lung resections), urology (nephrectomy), bariatric surgery, and even plastic surgery, where its precision is valued in procedures like facelifts and breast reductions.
Comparative Analysis: Harmonic vs. Other Surgical Energy Devices
To understand the value of the Harmonic Scalpel, it’s important to compare it with other energy-based surgical tools. Each device operates differently, offering specific benefits and drawbacks. Surgeons choose instruments strategically, based on procedural needs and anatomical challenges.
A Head-to-Head Comparison
This table provides a high-level breakdown for surgeons, engineers, and OR staff to understand the key differentiators between the primary surgical energy modalities.
| Technology | Mechanism | Key Advantages | Key Limitations | Best For… |
|---|---|---|---|---|
| Harmonic Scalpel | Ultrasonic Vibration (55.5 kHz) denatures protein at low temperatures (50-100°C). | Minimal lateral thermal spread; less surgical smoke; no electrical current passes through the patient; multifunctional (cuts and coagulates simultaneously). | Higher initial instrument cost; can be slower than monopolar for rapid, bulk tissue dissection; blade can be less maneuverable in some tight spaces. | Precise dissection near critical structures (nerves, vessels); minimally invasive surgery; patients with pacemakers. |
| Monopolar Electrocautery | High-frequency electrical current flows from an active electrode, through the patient’s body, to a large return pad. High heat (150-400°C). | Very fast for cutting and coagulation; versatile with multiple tip options; low instrument cost. | Significant lateral thermal spread; produces copious smoke; risk of alternate site burns from faulty return pad; current passes through patient, posing risk for pacemakers. | Rapid cutting and coagulation of large tissue areas in open surgery where precision near delicate structures is less critical. |
| Bipolar Electrocautery | Current flows only between the two tips of the instrument (e.g., forceps), confining energy to the tissue held between them. | Highly focused energy application; excellent for precise hemostasis; much safer than monopolar as current does not traverse the patient’s body. | Primarily a coagulation tool, not an effective cutting instrument. Limited to the tissue that can be grasped. | Sealing individual blood vessels; precise point coagulation in neurosurgery or other delicate fields. |
| Advanced Bipolar (e.g., LigaSure) | Uses bipolar energy combined with a feedback-controlled system that applies optimal pressure and energy to fuse vessel walls. | Creates exceptionally strong, reliable, and consistent vessel seals, often on vessels up to 7mm. Very efficient for ligating vascular pedicles. | Primarily a sealing and transecting device; less effective for the fine, painting-style dissection that the Harmonic excels at. | Vessel-rich structures like the splenic or renal pedicle; efficient ligation of vascular bundles without the need for sutures or clips. |
The Cost-Effectiveness Debate
The higher price of single-use Harmonic Scalpel handpieces often raises questions about value. However, growing economic evidence supports its cost-effectiveness. The key is evaluating total procedural cost—not just device price. Since OR time is among the most expensive hospital resources, shorter surgeries can offset the initial cost.
A 2018 systematic review in ClinicoEconomics and Outcomes Research analyzed 13 RCTs across procedures like gastrectomy, thyroidectomy, and colectomy. The results were compelling:
“As compared to conventional methods, Harmonic devices reduced total procedure costs by 8.7% (p=0.029), resulting in an absolute reduction of US$227.77 from mean conventional technique costs, derived primarily from a reduction in operating time costs.” (Cheng et al., 2018)
When isolating operating time costs, the review found an average savings of $544 per procedure. This highlights a strong value proposition: investing in advanced tools like the Harmonic Scalpel can achieve cost neutrality—or even savings—while also improving clinical outcomes.
For the Operating Room Team: A Practical Guide for Nurses and Technicians
The safe and efficient use of the Harmonic Scalpel is a team effort. The circulating nurse, scrub nurse, and surgical technologist play vital roles in the setup, intraoperative management, and troubleshooting of the system. A clear understanding of the device is essential for seamless surgical flow and patient safety.
Pre-Operative Setup & Safety Checklist
Before the procedure begins, a systematic check ensures the equipment is ready and functional. This process should be part of the standard operating procedure.
- Inspect Components: Visually inspect the generator for any damage. Check the integrity of the power cord, foot pedal, and the reusable handpiece cable. Ensure all components are clean and dry.
- Connect Securely: Plug the generator into a suitable power outlet. Connect the handpiece cable to the correct port on the generator. Connect the foot pedal if it is being used.
- Prepare the Sterile Field: The single-use sterile blade/instrument is passed to the scrub person. Aseptically connect the instrument to the non-sterile handpiece, ensuring it is fully seated and “clicks” into place. This connection is a common point of failure if not done correctly.
- Perform System Test: Before passing the assembled instrument to the surgeon, activate the test function. Most generators have a dedicated test button or sequence. This confirms the integrity of the entire system, from generator to blade tip. A successful test tone or visual indicator confirms readiness.
- Verify Settings: Verbally confirm the power settings with the surgeon. The generator typically has a minimum and maximum power level (e.g., levels 1-5). The surgeon will select a level based on the type of tissue being dissected and the desired effect (more coagulation vs. faster cutting).
Intraoperative Support & Troubleshooting
During the surgery, the OR team must be prepared to address common issues quickly and efficiently.
- Common Issue: Ineffective Cutting or Coagulation.
- Possible Causes: The most common cause is technique-related, such as insufficient tissue tension applied by the surgeon. Other causes include an accumulation of eschar (charred tissue) on the blade, or an incorrect power level for the tissue type.
- Solution: The scrub person should be ready with a sterile, moist sponge (like a Ray-Tec) to gently wipe the blade clean when the surgeon presents it. The circulating nurse can assist by confirming the power setting on the generator and adjusting it if requested by the surgeon.
- Possible Causes: The most common cause is technique-related, such as insufficient tissue tension applied by the surgeon. Other causes include an accumulation of eschar (charred tissue) on the blade, or an incorrect power level for the tissue type.
- Common Issue: System Alarm or Error Code.
- Possible Causes: This indicates a fault in the system. It could be a loose connection between the handpiece and the generator, a fault within the disposable blade, or a more serious issue with the handpiece or generator itself.
- Solution: The first step is to immediately and systematically check all connections. If the alarm persists after re-seating the connections, the disposable blade is the next most likely culprit and may need to be replaced. If a new blade does not resolve the issue, the handpiece or generator may be at fault, and a backup unit should be made available.
- Possible Causes: This indicates a fault in the system. It could be a loose connection between the handpiece and the generator, a fault within the disposable blade, or a more serious issue with the handpiece or generator itself.
Frequently Asked Questions (FAQs)
Q1: Will the Harmonic Scalpel completely replace traditional electrocautery?
A:Unlikely. It is more accurate to view them as complementary tools in a surgeon’s armamentarium. Monopolar electrocautery remains an extremely fast, versatile, and cost-effective tool for many applications, particularly in open surgery for bulk dissection where its thermal spread is less of a concern. The Harmonic Scalpel is a premium instrument, strategically chosen for procedures where its specific advantages—precision, minimal thermal injury, and safety in confined spaces—provide a distinct clinical benefit that justifies its cost. The choice is driven by the specific needs of the patient and the procedure.
Q2: How safe is the Harmonic Scalpel for the patient compared to other energy devices?
A:It is considered very safe, primarily due to two key factors. First, its mechanism of action does not involve passing any electrical current through the patient’s body. This completely eliminates the risks associated with monopolar electrocautery, such as grounding pad burns or electrical interference with cardiac implantable electronic devices (CIEDs) like pacemakers and defibrillators. Second, its lower operating temperature and focused energy delivery result in minimal lateral thermal damage, protecting adjacent healthy tissues (ScienceDirect, Parotidectomy Meta-Analysis). However, it is crucial to remember that it is still an energy device. Improper use, such as prolonged activation on a single spot or accidental contact with non-target tissue, can still cause unintended thermal injury.
Q3: Why do some studies show conflicting results on its benefits, with some finding no significant difference?
A:This is a common and important observation in the evaluation of any surgical technology. The variation in study results is often due to what researchers call “heterogeneity.” This can arise from several sources:
Surgeon Experience (Learning Curve):A surgeon highly proficient with conventional techniques but new to the Harmonic Scalpel may not initially see a time benefit.
Procedural Differences: The benefits may be more pronounced in complex, vessel-rich procedures than in simpler, more straightforward ones. For example, a study on uncomplicated laparoscopic cholecystectomy found no significant difference in operative time compared to electrocautery in the hands of experienced surgeons (PMC, Laparoscopic Cholecystectomy Study).
Patient Population:The advantages might be greater in patients with comorbidities (e.g., on blood thinners) where meticulous hemostasis is more critical.
Outcome Measurement:Different studies may measure outcomes like “blood loss” or “pain” in slightly different ways, making direct comparison difficult.
This is why large-scale systematic reviews and meta-analyses, which pool data from many studies, are so valuable. They help to smooth out the noise from individual trials and reveal the overall trend, which, for the Harmonic Scalpel, consistently points toward significant benefits over conventional methods (PMC, Umbrella Review 2023).
Conclusion: The Future of Surgical Dissection is Ultrasonic
The Harmonic Scalpel has become a cornerstone of modern surgical practice. Once considered niche, it is now a standard in many complex procedures. Its value lies in a powerful combination of benefits that directly tackle key surgical challenges:
- Precision: It offers unparalleled capability for fine, meticulous dissection with minimal collateral thermal damage, preserving function and promoting faster healing.
- Safety: By eliminating the flow of electricity through the patient and producing less surgical smoke, it enhances safety for both the patient and the entire surgical team.
- Efficiency: The elegant integration of cutting and coagulation into a single, fluid motion reduces intraoperative blood loss, shortens valuable operating time, and can lead to improved postoperative recovery and lower overall costs.
The evolution of ultrasonic surgical technology is ongoing. Future devices will likely feature advanced sensors and real-time energy modulation based on tissue characteristics. Continued miniaturization and improved articulation will enhance their role in robotic and single-port surgery. The Harmonic Scalpel is just the beginning of a broader wave of innovation—paving the way for safer, more precise, and more efficient surgical care.
The evolution of ultrasonic surgical tools like the Harmonic Scalpel reflects a broader trend in MedTech—toward smarter, data-driven solutions. As explored in our article on Generative AI in Healthcare, the integration of real-time data, feedback systems, and AI-driven insights is reshaping the surgical landscape. Together, these technologies promise a future of safer, faster, and more personalized surgical care.