The Hidden Danger: Why Recognizing Early Signs of Heart Attack is Crucial
When most people imagine a heart attack, they picture a dramatic, chest-clutching collapse like in the movies. But in reality, the early signs of heart attack are often far more subtle—and dangerously easy to ignore. A heart attack, or myocardial infarction, occurs when blood flow to a section of the heart muscle is severely reduced or completely blocked, typically by a clot forming over a ruptured plaque in a coronary artery (Mayo Clinic). The longer this blockage continues without treatment, the more damage is inflicted on the heart muscle.
The alarming truth? Many heart attacks begin with vague or mild symptoms—unexplained fatigue, discomfort, indigestion—that people often brush off as minor issues. These overlooked early signs of heart attack can lead to devastating consequences when medical care is delayed. Acting early can make the difference between survival, recovery, or irreversible damage.
Table of Contents
The “It’s Probably Nothing” Trap: Why We Overlook Critical Heart Clues
Why do so many people miss these vital signals from their bodies? Several factors contribute to this dangerous oversight:
- The Myth of the “Hollywood Heart Attack”: Popular culture often portrays heart attacks as sudden, crushing chest pain. When symptoms are different – like unexplained fatigue, nausea, or discomfort in the jaw or back – a heart attack isn’t the first, or even second, thought for many.
- “Silent” Myocardial Infarction (SMI): A significant portion of heart attacks are “silent,” meaning they occur with minimal, unrecognized, or no symptoms at all. Estimates from sources like the American Heart Association suggest that of the estimated 805,000 heart attacks each year in the U.S., around 170,000 are silent. In India, the situation is particularly concerning, with some reports indicating that silent or asymptomatic heart attacks could account for up to 45-50% of all cardiac events (Pune Cardiologist citing research, Hindustan Times quoting Dr. Hiremath). These are often discovered accidentally during routine check-ups later, after irreversible damage may have already occurred.
- Misattribution is Common: It’s human nature to seek simple explanations for discomfort. Unusual tiredness is easily blamed on a busy week, shortness of breath on being unfit, or indigestion on a recent heavy meal. Our brains try to rationalize symptoms, often overlooking potentially serious underlying causes.
- The Danger of Delay: “Time is Muscle.” This critical phrase in cardiology emphasizes that every minute blood flow to the heart is blocked, more heart muscle is damaged or dies (Cleveland Clinic). Recognizing early signs and seeking immediate medical help is paramount to minimizing damage and improving chances of survival and quality of life post-event.
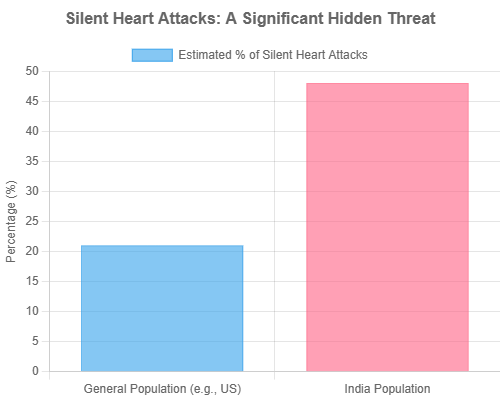
Figure 1: Estimated Percentage of Silent Myocardial Infarctions (SMI).
The Core: 10 Early Warning Signs of a Heart Attack Most People Ignore
These signs can appear hours, days, or even weeks before a major heart attack. They can be persistent or intermittent. Pay close attention, especially if they are new, unexplained, or unusual for you. Remember, you might not experience all of them, and symptoms can vary significantly between individuals, and particularly between men and women.
1. Unusual or Extreme Fatigue
- What it Feels Like: A profound and overwhelming sense of exhaustion that isn’t relieved by rest. This isn’t your usual tiredness after a long day—it’s a debilitating lack of energy that makes even simple daily activities feel like monumental tasks. For many, this is one of the early signs of a heart attack, often overlooked.
- The Medical Lowdown: When coronary arteries narrow due to atherosclerosis (plaque buildup), the heart receives less oxygen-rich blood. This forces the heart muscle to work harder to pump blood throughout the body, leading to significant fatigue (St. Vincent’s Health System). The body may also divert blood from less vital organs (like limbs) to the heart and brain, further contributing to a generalized feeling of tiredness.
- Why It’s Ignored: Fatigue is a vague and non-specific symptom, frequently brushed off as a result of poor sleep, stress, viral illness, overwork, or simply aging—making it easy to miss as one of the early signs of heart attack.
- Spotlight on Specific Groups:
- Women: This is one of the most common prodromal (early warning) symptoms reported by women, sometimes occurring for days or even weeks leading up to a heart attack (CDC on women’s symptoms).
- Diabetics: Nerve damage (diabetic neuropathy) can blunt or alter typical pain signals. As a result, fatigue might be a more prominent, or even the only, warning sign of cardiac distress in individuals with diabetes.
- An Indian Story: Anuraj Singh, a 21-year-old from India, experienced a major heart attack. While his more acute symptoms leading to hospitalization were back pain and chest tightening, his preceding period was marked by intense stress, erratic meals, and “sleepless nights” which contributed to an overall unhealthy state and systemic fatigue, putting immense strain on his heart (Indian Express – Anuraj Singh Story). Many individuals in high-stress jobs in India report chronic fatigue, often ignoring it until a critical event occurs.
- Data Point: Studies show a significant percentage of women report persistent fatigue, sleep issues, and breathlessness for weeks before their heart attacks—classic yet overlooked early signs of a heart attack (Cleveland Clinic on women’s symptoms).
- Action Now: If you experience new, unexplained, persistent, or severe fatigue that significantly interferes with your daily life, consult your doctor. Don’t just try to “push through it.”
2. Subtle Chest Discomfort (Pressure, Squeezing, Fullness)
- What it Feels Like: This is often not the sudden, intense, crushing pain depicted in movies. It can manifest as a milder pressure, tightness, squeezing, aching, burning, or a feeling of fullness, typically in the center or left side of the chest (CDC). The discomfort might last for several minutes, or it may come and go (intermittent).
- The Medical Lowdown: This sensation is the hallmark symptom of ischemia – the heart muscle isn’t receiving enough oxygen-rich blood, usually due to a blocked or significantly narrowed coronary artery. The discomfort arises from the heart muscle cells sending out distress signals.
- Why It’s Ignored: If the discomfort isn’t severe, or if it’s intermittent, people might readily dismiss it as heartburn, indigestion, gas, or a pulled muscle. The statement “It’s not chest pain, it’s pressure” is one that cardiologists hear often and take very seriously (St. Vincent’s Health System).
- An Indian Story: Abhijeet Kadam, a 28-year-old in Mumbai, experienced chest pain radiating to his left hand before his heart attack (Wockhardt Hospitals – Abhijeet Kadam Story). Anuraj Singh, the 21-year-old, felt a “tightening of his chest,” which, combined with back pain, prompted him to seek help, though initially, even medical professionals considered antacids (Indian Express – Anuraj Singh Story).
- Data Point: While chest pain or discomfort is the most common symptom of a heart attack, its nature can vary widely. Many individuals, especially women, may experience atypical chest sensations or even no chest discomfort at all.
- Action Now: Any new or unexplained chest discomfort, regardless of its intensity, especially if it recurs or is associated with exertion or stress, warrants immediate medical attention. If it’s severe or accompanied by other symptoms like shortness of breath or sweating, call emergency services without delay.
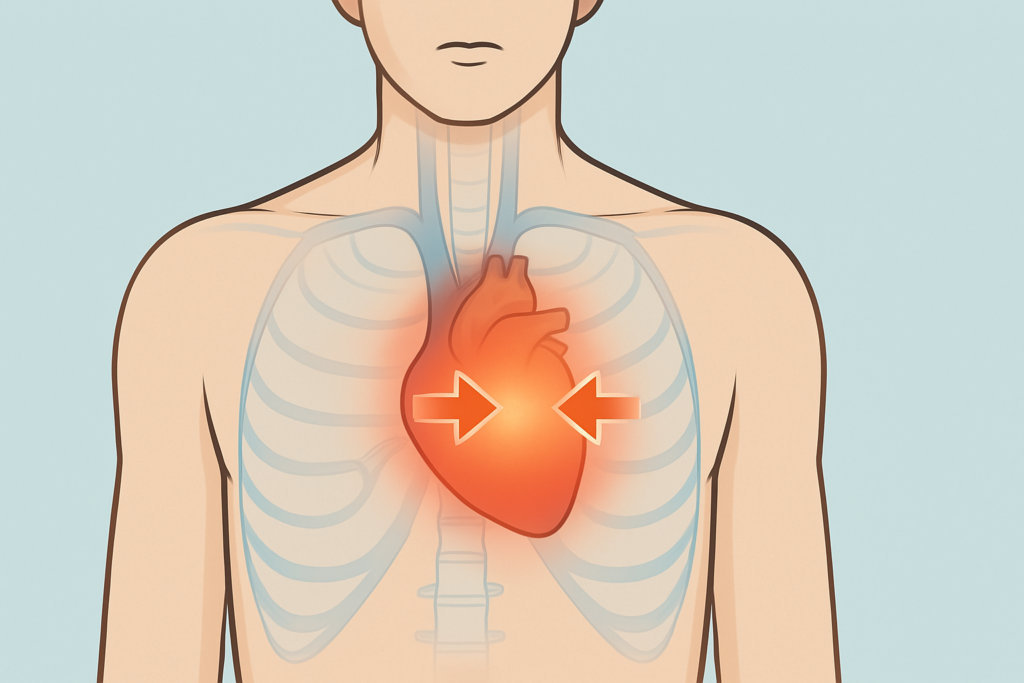
3. Pain/Discomfort in Other Upper Body Areas (One or Both Arms, Back, Neck, Jaw, Stomach)
- What it Feels Like: Pain or discomfort that isn’t localized to the chest but can radiate from it or appear independently in the shoulders, arms (often the left, but can affect both), neck, jaw, back (commonly between the shoulder blades), or the upper part of the stomach (CDC).
- The Medical Lowdown: This phenomenon is known as “referred pain.” The nerves that carry signals from the heart share pathways in the spinal cord with nerves from these other upper body areas. The brain can misinterpret the pain signals originating from the heart as coming from these other, more commonly experienced, locations.
- Why It’s Ignored: Such pain is very easily mistaken for more common ailments like a pulled muscle, dental problems (jaw pain), arthritis in the neck or shoulder, or general aches and pains from daily activities.
- Spotlight on Specific Groups:
- Women: Women are more likely than men to experience atypical pain, such as in the back, jaw, or neck, sometimes without any obvious chest discomfort (Mayo Clinic on women’s symptoms).
- An Indian Story: Anuraj Singh, the 21-year-old survivor, reported “shooting back pain” as one of his alarming symptoms that led him to the hospital before he collapsed (Indian Express – Anuraj Singh Story). Dr. Sumeet Sethi from Max Super Speciality Hospital, Saket, notes that women can develop pain in the jaw, neck, or back (Biospectrum India).
- Action Now: If you experience unexplained pain or discomfort in these upper body areas, especially if it’s new, occurs with exertion, is accompanied by other potential heart attack symptoms, or doesn’t resolve with usual remedies for muscle pain, seek medical advice promptly.
Image Suggestion: Body outline highlighting common areas of referred pain during a heart attack – arms, jaw, neck, back, stomach.Pain from a heart attack can “refer” to other parts of the upper body.
4. Shortness of Breath (Dyspnea)
- What it Feels Like: Difficulty breathing, feeling like you can’t get enough air into your lungs, or a sensation of breathlessness. This can occur with or without accompanying chest discomfort. It might happen during physical activity, while at rest, or even wake you from sleep (American Heart Association).
- The Medical Lowdown: If the heart isn’t pumping blood efficiently due to a blockage, blood can back up in the pulmonary veins and leak fluid into the lungs (a condition called pulmonary congestion or edema). This fluid in the air sacs makes it difficult to breathe. Additionally, the heart muscle itself not getting enough oxygen can trigger a reflex sensation of breathlessness.
- Why It’s Ignored: Breathlessness is often attributed to being out of shape, having asthma, allergies, anxiety, a common cold or respiratory infection, or even just the effects of aging.
- Data Point: For some—particularly older adults or people with diabetes—shortness of breath may be the only symptom of a heart attack. It can even appear before chest discomfort, making it a critical early sign of heart attack that shouldn’t be overlooked (CDC).
- Action Now: Sudden or unexplained shortness of breath, especially if it’s new, worsening, occurs with minimal exertion, or is accompanied by other symptoms, requires urgent medical evaluation.

5. Dizziness, Lightheadedness, or Fainting (Syncope)
- What it Feels Like: A sensation of feeling woozy, unsteady, as if you’re about to pass out (presyncope), or briefly losing consciousness (syncope). While often overlooked, these episodes can be among the early signs of heart attack, particularly in certain individuals.
- The Medical Lowdown: A damaged heart muscle due to a heart attack, or an arrhythmia (an abnormal heart rhythm) triggered by the cardiac event, can reduce the heart’s ability to pump blood effectively. This can lead to a temporary decrease in blood flow and oxygen supply to the brain, causing dizziness or fainting (Mayo Clinic).
- Why It’s Ignored: TThese symptoms are frequently dismissed as harmless side effects of dehydration, low blood sugar, quick posture changes (orthostatic hypotension), or inner ear issues. However, when unexplained, they may be critical early signs of heart attack, especially when linked with other subtle symptoms.
- Action Now: Any unexplained episode of dizziness, lightheadedness, or fainting should always be investigated by a doctor. If it’s sudden, severe, or accompanied by other potential heart attack symptoms, call emergency services immediately.
6. Nausea or Vomiting
- What it Feels Like: A sudden onset of nausea, the urge to vomit, or actual vomiting—sometimes without any obvious digestive cause. While these symptoms might seem routine, they can be among the early signs of heart attack, especially when paired with other subtle indicators.
- The Medical Lowdown: The heart’s distress signals during an attack can stimulate the vagus nerve, a long nerve that connects the brain to various organs, including the heart and the digestive system. This stimulation can trigger feelings of nausea and lead to vomiting. This is particularly common with heart attacks affecting the inferior (bottom) wall of the heart, as this part is anatomically close to the diaphragm and stomach (Cleveland Clinic).
- Why It’s Ignored: These symptoms are commonly attributed to less serious issues such as food poisoning, a stomach bug, indigestion, or even stress. Because nausea and vomiting are so widespread and non-specific, they’re often dismissed and not recognized as early signs of heart attack.
- Spotlight on Specific Groups:
- Women: Women tend to experience nausea and vomiting as a heart attack symptom more frequently than men (Goshen Health).
- Action Now: If nausea or vomiting appears suddenly, is unexplained, and is accompanied by other possible early signs of heart attack—like chest discomfort, shortness of breath, or cold sweating—seek immediate medical care. Ignoring these symptoms could delay life-saving treatment.
7. Breaking Out in a Cold Sweat (Diaphoresis)
- What it Feels Like: A sudden episode of intense sweating—cool and clammy skin, often without any heat, exertion, or clear reason. This unexpected cold sweat can appear even while resting and is often reported as one of the early signs of heart attack.
- The Medical Lowdown: During a heart attack, the body’s sympathetic nervous system (responsible for the “fight or flight” response) is often activated due to the stress of the event and the body’s attempt to maintain blood flow to vital organs. This activation can cause widespread sweating (diaphoresis) as a physiological response (CDC).
- Why It’s Ignored: Cold sweats are often dismissed as signs of anxiety, panic attacks, hormonal fluctuations (such as hot flashes during menopause), or the onset of fever or flu—causing many to overlook this symptom as one of the subtle early signs of heart attack.
- Action Now: Unexplained cold sweats, especially when occurring suddenly and accompanied by any other warning sign from this list (like chest discomfort, nausea, or dizziness), are a significant red flag and warrant immediate emergency medical help.
8. Indigestion, Heartburn-like Symptoms, or Stomach Pain
- What it Feels Like: A burning sensation in the chest or upper abdomen, belching, bloating, fullness, or general stomach discomfort—often mistaken for indigestion or acid reflux. These symptoms can closely resemble common digestive issues but may also be early signs of heart attack.
- The Medical Lowdown: The heart is located in close proximity to the esophagus and stomach. Due to shared nerve pathways (similar to referred pain), pain or discomfort originating from the heart, especially an inferior wall myocardial infarction (affecting the bottom part of the heart), can be perceived as gastrointestinal distress (Cleveland Clinic notes people often think it’s indigestion).
- Why It’s Ignored: Heartburn, indigestion, and gas are extremely common and typically linked to food, stress, or minor digestive issues. Most people treat them with over-the-counter antacids and move on—often overlooking that these can be early signs of heart attack, especially when they present differently than usual.
- An Indian Story: Anuraj Singh, the 21-year-old heart attack survivor, had experienced “intense gas bouts a week before” and some chest pain. When he initially visited a doctor for his chest pain, he was prescribed antacids and advised to get an ECG the next day, highlighting how easily these symptoms can be misattributed, even by medical professionals in the initial stages without further investigation (Indian Express – Anuraj Singh Story).
- Action Now: If you feel a burning sensation or stomach discomfort that seems unusual, more intense than normal, unresponsive to typical remedies, or paired with other symptoms (sweating, breathlessness, or chest pressure), don’t ignore it. What seems like indigestion may be one of the early signs of heart attack. Prompt medical attention can make all the difference.
9. Sleep Disturbances
- What it Feels Like: New or unusual difficulty falling asleep (insomnia), frequent awakenings during the night, or waking up feeling anxious and unrested—even after spending several hours in bed. These disruptions might not seem alarming at first but can be subtle early signs of heart attack.
- The Medical Lowdown: Sleep disturbances can be linked to underlying anxiety or stress that may precede a cardiac event. More directly, physical discomfort such as nocturnal angina (chest pain that occurs at night, often waking the person) or orthopnea (shortness of breath when lying flat, forcing the person to sit up to breathe) can severely disrupt sleep patterns. These are signs the heart is struggling.
- Why It’s Ignored: Most people associate sleep problems with work stress, lifestyle choices, caffeine, or poor sleep hygiene. Because sleep disturbances are so common, they’re rarely linked to serious cardiac conditions and are often overlooked as early signs of heart attack.
- Spotlight on Specific Groups:
- Women: Women are more likely than men to report experiencing sleep disturbances in the weeks or months leading up to a heart attack (Cleveland Clinic on women’s pre-attack symptoms).
- An Indian Story: Anuraj Singh’s “sleepless nights” were part of a broader pattern of intense stress and unhealthy lifestyle habits that ultimately culminated in his heart attack (Indian Express – Anuraj Singh Story). While his sleeplessness was tied to severe stress, it underscores how the body being under duress can manifest in disrupted sleep, which itself can be a risk factor or an overlooked symptom cluster.
- Action Now: Persistent, unexplained changes in your sleep patterns, especially if accompanied by increased daytime fatigue, anxiety, or any other symptoms from this list, should be discussed with your doctor.
10. Unexplained Anxiety or a Sense of Impending Doom
- What it Feels Like: A sudden, overwhelming wave of anxiety, nervousness, or an intense premonition that something terrible is about to happen—often described as a “sense of impending doom.” This can arise without any apparent reason or external stressor and may be one of the more overlooked early signs of heart attack.
- The Medical Lowdown: The body’s acute stress response during a significant physiological crisis like a heart attack can trigger intense feelings of anxiety. Some researchers also theorize that the body, at a very primal level, can sometimes sense a life-threatening internal change, manifesting as profound unease or fear.
- Why It’s Ignored: These feelings are frequently chalked up to panic attacks, chronic anxiety, or psychological stress—especially in individuals with a history of mental health issues. However, when these emotions occur abruptly and intensely, they may actually be early signs of heart attack, not just emotional distress.
- Action Now: While anxiety can have many causes, if it is sudden, severe, unexplained, and particularly if it is accompanied by any other physical symptoms from this list (like chest discomfort, shortness of breath, or dizziness), it should not be dismissed and warrants urgent medical attention.
The Indian Heart: A Unique Set of Challenges
Heart disease in India isn’t just a statistic; it’s a rapidly growing epidemic with distinct characteristics that demand special attention. Understanding these nuances is crucial for both public health strategies and individual awareness.
- The Rising Tide & Younger Onset: India bears one of the highest burdens of cardiovascular disease (CVD) globally. According to the World Health Organization (WHO), in 2016, CVDs accounted for 27% of total deaths due to Non-Communicable Diseases (NCDs) in India and 45% of deaths in the 40-69 year age group. Alarmingly, the Indian Heart Association (IHA) highlights that 50% of all heart attacks in Indian men occur under 50 years of age, and a staggering 25% occur under 40 years of age. This indicates that heart disease often strikes Indians a decade or more earlier than their Western counterparts.
- Why India? Unique Risk Factors:
- Genetic Predisposition: South Asians, including Indians, are known to have a genetic predisposition to developing heart disease. This includes factors like having smaller coronary arteries and a higher tendency towards metabolic syndrome (a cluster of conditions including increased blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol or triglyceride levels) (IHA).
- Lifestyle Shifts: Rapid urbanization and economic changes have led to significant lifestyle shifts. These include dietary changes towards more processed foods, higher intake of unhealthy fats and sugars, increased sedentary behavior due to desk jobs and motorized transport, and high levels of chronic stress, particularly in demanding urban professions (Wockhardt Hospitals on lifestyle).
- High Prevalence of Co-morbidities: India is often referred to as the “diabetes capital of the world” (IHA). The high prevalence of diabetes, often undiagnosed or poorly managed, significantly elevates heart attack risk. Similarly, high rates of hypertension (high blood pressure) and dyslipidemia (abnormal cholesterol levels) are major contributors to the CVD burden.
- The “Silent” Epidemic in India: As previously mentioned, a substantial percentage of heart attacks in India are silent or present with atypical symptoms. Estimates suggest this could be as high as 45-50% of all cardiac events (Pune Cardiologist, Hindustan Times). This makes early detection even more challenging and is often compounded by lower awareness levels about these subtle signs in some segments of the population..
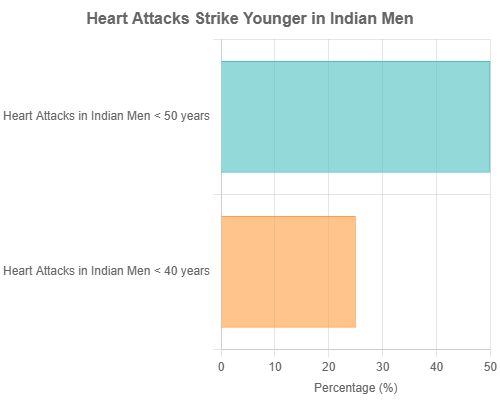
Figure 2: Percentage of Heart Attacks in Indian Men Occurring Below Certain Ages (Source: Indian Heart Association).
Key Takeaways: The Indian Context
- Heart attacks in India often occur at a younger age.
- A combination of genetic factors, lifestyle changes, and high rates of diabetes/hypertension contribute to this.
- A high percentage of heart attacks may be “silent” or present with atypical symptoms, demanding greater awareness.
Did you know that a defibrillator is a life-saving device used to restore a normal heartbeat during cardiac arrest? To learn more about how defibrillators work and when they’re used, click here.
“Is This It?” – Recognizing the Red Flags and Acting Fast
Knowing the warning signs is the first crucial step, but recognizing them in yourself or someone else and then acting decisively is what truly saves lives. Here’s how to navigate this critical juncture:
- Trust Your Gut Feeling: If something feels “off,” new, different, or just not right for your body, don’t ignore it. You are the best judge of your own body. Even if a symptom seems vague, if it’s persistent or worrying, it’s worth investigating.
- It’s Not Always Dramatic: Remember, heart attack symptoms can be mild, subtle, or intermittent (come and go). Don’t wait for the “Hollywood heart attack” with debilitating, crushing chest pain before you take action. Many people who have had heart attacks report that their symptoms were not what they expected.
- When to Consult Your Doctor (Non-Emergency): If you experience any of the warning signs and they are new, persistent, or worrying, but not acutely severe or life-threatening at that moment, make an appointment to see your doctor promptly. This is especially true for symptoms like ongoing unusual fatigue, intermittent mild discomfort, or gradual changes in your exercise tolerance.
- When to Call Emergency Services (e.g., 102/108 in India or your local emergency number) IMMEDIATELY:
- Sudden, severe, or persistent chest pain, pressure, squeezing, or discomfort (especially if it lasts more than a few minutes or goes away and comes back).
- Pain or discomfort spreading from the chest to the arm(s) (especially the left), jaw, neck, or back.
- Sudden or severe shortness of breath, occurring at rest or with minimal exertion.
- Sudden unexplained dizziness, lightheadedness, or actual fainting.
- Breaking out in a cold sweat for no apparent reason.
- A combination of these symptoms, even if some are mild.
- The Golden Hour: The first hour after the onset of heart attack symptoms is often referred to as the “golden hour.” Prompt medical treatment, such as angioplasty or thrombolytic therapy (clot-busting drugs), within this timeframe can significantly reduce heart muscle damage and dramatically improve chances of survival and recovery (Biospectrum India on timely action). Every minute counts.
- What to Do While Waiting for Help:
- Call Emergency Services First: This is the most important step. Do not attempt to drive yourself or the person to the hospital unless explicitly instructed by emergency services, as they can provide life-saving treatment en route.
- Chew Aspirin (if advised and appropriate): Emergency dispatchers may advise the person to chew one adult-strength (300-325mg) aspirin, provided they are not allergic and have no medical conditions (like active bleeding or on certain medications) that would make it unsafe. Aspirin helps by inhibiting blood clotting.
- Stay Calm and Rest: Help the person sit or lie down in a comfortable position. Loosen any tight clothing. Try to remain as calm as possible.
Beyond the Alarms: Building a Heart-Healthy Future
While recognizing early warning signs is crucial for immediate, life-saving action, the journey to heart health extends far beyond emergency response. Long-term well-being relies on proactive prevention and management of risk factors. Here are key strategies:
- Know Your Numbers: Ignorance is not bliss when it comes to heart health. Regularly monitor and understand your key health indicators:
- Blood Pressure: Aim for levels below 120/80 mmHg. High blood pressure often has no symptoms but is a major risk factor.Cholesterol Levels (Lipid Profile): Pay attention to total cholesterol, LDL (“bad”) cholesterol, HDL (“good”) cholesterol, and triglycerides. Work with your doctor to understand your targets.Blood Sugar (Fasting Glucose & HbA1c): Essential for everyone, but especially critical if you have diabetes or prediabetes. Good blood sugar control reduces cardiovascular risk.Body Mass Index (BMI) and Waist Circumference: Maintaining a healthy weight reduces strain on the heart.
- The Power of Prevention – Embrace a Heart-Healthy Lifestyle:
- Diet: Focus on a diet rich in fruits, vegetables, whole grains, lean protein (fish, poultry, legumes), and healthy fats (nuts, seeds, olive oil). Limit processed foods, sugary drinks, excessive salt, red meat, and unhealthy trans and saturated fats (Wockhardt Hospitals – Healthy Diet).
- Exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise (like brisk walking, cycling, swimming) or 75 minutes of vigorous-intensity exercise per week, plus muscle-strengthening activities on two or more days a week.
- Quit Smoking: Smoking is one of the most significant risk factors for heart disease. If you smoke, seek help to quit. The benefits begin almost immediately.
- Limit Alcohol: If you drink alcohol, do so in moderation.
- Manage Stress: Chronic stress can contribute to heart disease. Practice stress-reducing techniques like yoga, meditation, deep breathing exercises, spending time in nature, or engaging in hobbies.
- Adequate Sleep: Aim for 7-8 hours of quality sleep per night. Poor sleep can contribute to risk factors like high blood pressure and obesity.
- Regular Check-ups and Screening: Visit your doctor for regular health screenings and check-ups. This is especially important if you have known risk factors such as a family history of heart disease, diabetes, hypertension, or high cholesterol. Early detection and management of these conditions can significantly lower your risk of a heart attack. Dr. Sanjeev Gera from Fortis Hospital, Noida, suggests that a basic heart screening test should be done in the 20s, particularly if one is a smoker or regular drinker (Indian Express – Dr. Gera’s advice).
Your Lifesaving Blueprint: Recognizing Early Signs of Heart Attack & Taking Decisive Action
This section offers a clear, actionable guide to identifying and responding to the early signs of heart attack, helping you take proactive control of your heart health and react swiftly in critical moments.
Understanding Your Body’s Signals: A Recap of Easily Missed Warnings
- Key Overlooked Symptoms: Be particularly vigilant for the following, as they are often dismissed or misattributed:
- Atypical chest discomfort: This isn’t always sharp pain; it can be pressure, fullness, squeezing, or even a burning sensation.
- Unexplained and persistent fatigue, weakness, or shortness of breath, especially if new or worsening with minimal exertion.
- Pain or discomfort in other areas: Jaw, neck, back (between shoulder blades), one or both arms (more commonly left), or the stomach.
- Symptoms mimicking indigestion, heartburn, or flu-like symptoms (nausea, cold sweat), especially if these are unusual for you, severe, or accompanied by other signs.
- Variability is Key: It’s crucial to remember that symptoms can differ significantly from person to person. What one individual experiences might be vastly different for another. Symptoms also vary notably between men and women. For instance, women are more likely to experience atypical symptoms like fatigue, nausea, and pain in the back or jaw, sometimes without significant chest discomfort (UTMB Health on women’s symptoms). Individuals with conditions like diabetes may experience fewer or no pain symptoms at all due to diabetic neuropathy (nerve damage), making non-pain symptoms like profound fatigue or shortness of breath even more critical to recognize.
- The Danger of “Silent” Attacks: Up to 45–50% of heart attacks in India are considered “silent,” showing little or no chest pain. These silent events can still cause severe heart damage and often go unrecognized until it’s too late. Remember:
“Just because there’s no pain doesn’t mean there’s no problem.” (Pune Cardiologist).
Your Personal Action Plan for Heart Health Awareness & Emergency Response
A proactive approach involves several phases, from self-awareness to emergency preparedness.
Phase 1: Heightened Self-Awareness & Risk Assessment
- Task 1.1: Know Your Personal Risk Profile.
- Execution Points: Honestly assess your family history of early heart disease (father/brother diagnosed <55 years, mother/sister <65 years). Identify your existing conditions like diabetes, high blood pressure, high cholesterol. Evaluate your lifestyle factors: smoking status, typical diet, level of physical activity, and chronic stress levels.
- Outcome: A clear understanding of your individual vulnerability. This knowledge empowers you to make targeted preventive lifestyle changes and discuss specific screening needs with your doctor.
- Task 1.2: Learn to Listen to Your Body’s Subtle Cues.
- Execution Points: Actively pay attention to any new, persistent, or unusual symptoms from the “10 Signs” list discussed earlier. Don’t immediately dismiss them. Create a mental (or even written) note of when they occur, what they feel like, what triggers them (e.g., exertion, stress, eating), and what makes them better or worse.
- Outcome: An increased ability to detect potential early warnings before they escalate into a major event. This self-awareness is your first line of defense.
Phase 2: Proactive Consultation & When to Escalate
- Task 2.1: Schedule and Attend Regular Health Check-ups.
- Execution Points: Don’t wait for symptoms to appear. Discuss your heart health and risk factors openly with your doctor during routine visits. Undergo recommended screenings such as blood pressure checks, cholesterol (lipid profile) tests, blood sugar tests (fasting and HbA1c), and an ECG if your doctor deems it necessary based on your risk profile.
- Outcome: Early detection of underlying conditions like hypertension, dyslipidemia, or diabetes. You’ll receive personalized medical advice and establish a baseline for your health, making it easier to spot significant changes later.
- Task 2.2: Differentiate Between Concern (Doctor Visit) and Crisis (Emergency Call).
- Execution Points:
- Concern (Consult Doctor Promptly): If you experience new, persistent, or gradually worsening symptoms like unusual fatigue lasting days or weeks, intermittent mild chest discomfort or pressure, unexplained changes in your sleep patterns, or recurring mild indigestion-like symptoms that are unusual for you and don’t resolve easily.
- Crisis (Call Emergency Services IMMEDIATELY – e.g., 102/108 in India): If you experience sudden severe chest pain or pressure (especially if lasting more than a few minutes or radiating), pain spreading to the arm/jaw/neck/back, sudden severe shortness of breath (especially at rest), fainting or near-fainting, breaking out in a cold sweat, or a sudden combination of acute, alarming symptoms.
- Outcome: Confidence in knowing the appropriate level of response. This ensures you receive timely care without either unnecessary panic for minor issues or dangerous delays for critical ones.
- Execution Points:
Phase 3: Emergency Preparedness & Action
- Task 3.1: Be Prepared for an Emergency.
- Execution Points: Save local emergency medical service numbers (e.g., 102, 108 in India) on your phone and keep them in a visible place at home. Know the location of the nearest hospital that is equipped for cardiac emergencies (has a cath lab). Inform family members and close friends about these warning signs and what to do.
- Outcome: Reduced panic and faster, more efficient action during a critical situation. Preparation can save precious minutes.
- Task 3.2: Act Decisively – Time Is Muscle.
- Execution Points: If you suspect you or someone else is having a heart attack, call emergency services immediately. Do not attempt to drive yourself or the person to the hospital unless specifically instructed by emergency services (they can start treatment en route and choose the best hospital). While waiting for help, if advised by the emergency dispatcher and there are no contraindications (like aspirin allergy or active bleeding problems), the person may be advised to chew one adult aspirin (300-325mg). Help the person rest in a comfortable position, usually sitting up.
- Outcome: Maximizing the chances of survival and minimizing long-term heart damage by accessing professional medical care as quickly as possible.
Key Principles for Survival: Don’t Delay, Don’t Deny
- Principle 1: Overcoming the “It Can’t Be Me” Syndrome.
- Action: Acknowledge that heart attacks can happen to anyone, regardless of age, perceived fitness level, or general health. Denial is a common psychological response but can be deadly when it comes to heart symptoms.
- Principle 2: The High Risk of Misattribution.
- Action: Be extremely cautious about dismissing potential heart attack symptoms as minor ailments (like indigestion, muscle strain, simple fatigue, or anxiety) without proper medical evaluation. This is especially true if the symptoms are new, severe, unusual for you, or occur in a pattern (e.g., with exertion).
What If Symptoms Are Vague or Unclear?
- Guidance: When it comes to early signs of heart attack, uncertainty is no excuse for inaction. Many symptoms—like fatigue, indigestion, or shortness of breath—can seem mild or unrelated. But if something feels “off” and you can’t explain it, it’s worth paying attention.
- The best approach? Always err on the side of caution. It’s far better to visit a healthcare provider and discover that nothing’s wrong than to ignore what could be a life-threatening warning. If you experience concerning symptoms—even if they don’t perfectly match the “classic” heart attack profile—don’t wait.
Key Takeaways: Your Action Blueprint
- Know your personal risk factors and listen to your body’s signals.
- Differentiate between symptoms needing a prompt doctor’s visit versus an immediate emergency call.
- In an emergency: Call for help first, then consider aspirin (if appropriate), and rest.
- Never dismiss persistent or worrying symptoms. When in doubt, get checked out.
Stay Informed, Stay Healthy: Your Journey Continues
Recognizing the early signs of heart attack isn’t just helpful—it’s potentially life-saving. Whether these symptoms are subtle or unexpected, they’re your body’s urgent signals that something serious may be happening. The key is not to dismiss or delay but to listen and act.
We urge you to share this knowledge with your loved ones—your family, friends, and coworkers. Awareness is the first and most powerful tool in preventing tragedy. A single conversation could lead to early diagnosis, timely treatment, and even a life saved.
Take charge of your health. Know the signs. Spread the word.
Your awareness could change someone’s future.
What are your thoughts on this? Have you or someone you know experienced any of these subtle or atypical warning signs? We invite you to share your experiences or ask questions in the comments section below. Your story could help others.
Don’t miss our upcoming posts where we’ll dive deeper into crucial aspects of heart health! Subscribe to our blog and follow us on social media to stay updated on topics such as “Simple Lifestyle Changes to Drastically Reduce Your Heart Attack Risk,” “Understanding Your Key Heart Health Numbers: What Your Doctor Looks For,” and “Navigating Life After a Heart Scare: Recovery and Prevention.”
Your heart health is largely in your hands. Be aware, be proactive, and be prepared. Your heart will thank you for it.
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.