Introduction
Breast cancer is the most common cancer in women globally and the second leading cause of cancer death in the U.S.[nationalbreastcancer.org][cancer.org]. About 1 in 8 women will develop invasive breast cancer, and 1 in 39 will die from it [cancer.org].. However, recognizing the early signs of breast cancer is critical — early detection raises the 5-year survival rate to 99%. Thanks to improved screening and treatment, over 4 million women in the U.S. have survived breast cancer.
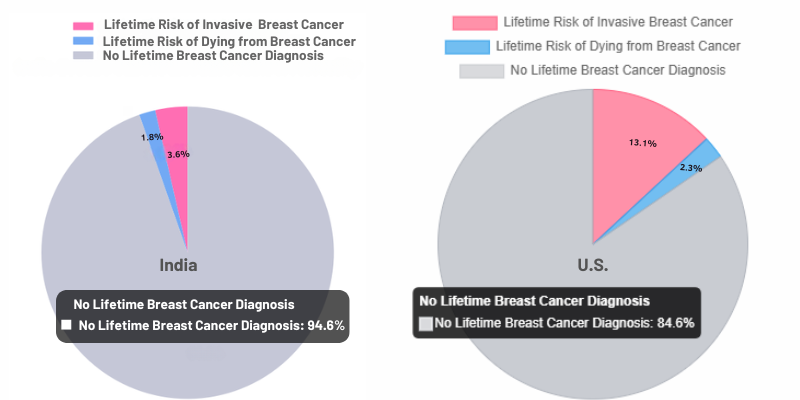
Breast Cancer Lifetime Risk & Mortality
Source:[cancer.org] [cancerindia.org.in]
This article explores the early signs of breast cancer—subtle symptoms that may appear before a tumor becomes obvious. You’ll learn what to watch and feel for, how to do a self-exam, and why early detection is so important. Whether you’re in your 20s or 60s, have a family history, or care for someone at risk, this guide will help you take charge of breast health with clear next steps and trusted resources.
Table of Contents
Common Early Signs and Symptoms of Breast Cancer
Breast cancer can appear differently in each person, and some women may notice no symptoms at all—early detection often happens through routine screenings like mammograms [cdc.gov]. However, when symptoms do occur, the early signs of breast cancer are usually subtle. That’s why knowing what’s normal for your body is essential. If you spot any unusual changes, speak with your doctor promptly. Below are the most common early signs to watch for:
- A new lump or mass in the breast or underarm: It is one of the most recognized early signs of breast cancer. While these lumps are often painless and hard with irregular edges, they can also feel soft, round, or tender[cancer.org]. Not all lumps are cancerous—many are benign—but any new lump should be evaluated by a healthcare provider[cdc.gov]. Lumps in the underarm area (axilla) may also suggest the cancer has spread to nearby lymph nodes.
- Thickening or swelling of part of the breast: You might notice an area of the breast feels thicker or firmer than the rest, even if you can’t clearly feel a distinct lump[cdc.gov]. Swelling can occur in part or all of the breast, sometimes without a palpable lump[cancer.org].
- Irritation or dimpling of the breast skin: It may resemble an orange peel texture (peau d’orange)[cdc.gov] and can be an early sign of breast cancer. This occurs when a tumor pulls on the skin’s supporting ligaments. Redness or irritation may also appear, particularly in cases of inflammatory breast cancer.
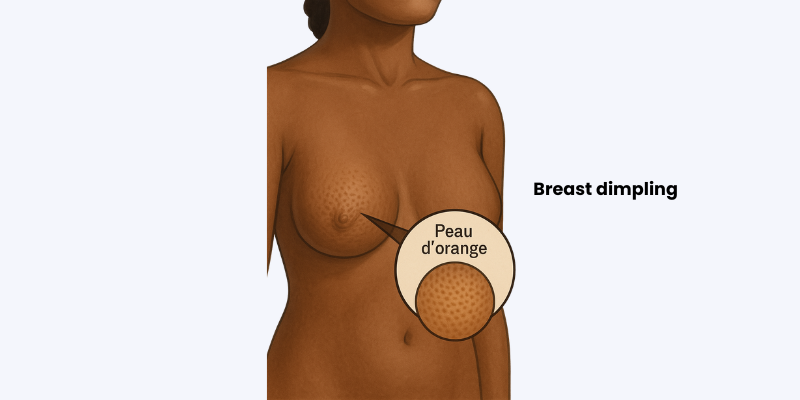
Medical illustration of breast dimpling, showing an orange peel-like skin texture
- Redness, scaliness, or flaky skin on the nipple or breast: Changes in the nipple area such as redness, dryness, flaking, or scaling of the nipple or areola can be an early sign[cdc.gov]. Paget’s disease of the breast, a rare type of cancer, often starts with such symptoms on the nipple[cdc.gov].
- Nipple changes or discharge: The nipple may turn inward (retract) or appear flattened instead of protruding normally[cdc.gov]. There may be pain or tenderness in the nipple area. Nipple discharge (other than breast milk) is another warning sign – especially if it’s bloody or clear and spontaneous[cdc.gov].
- Any change in the size or shape of the breast: One breast may become noticeably larger or lower than the other, or you may observe a change in breast contour[cdc.gov]. This could be due to a tumor deep in the breast tissue pushing outward.
- Pain in any area of the breast: Although many breast cancers are painless, some women do feel pain or tenderness in the breast or nipple[cdc.gov]. Pain alone is less common as an early sign than the other changes listed, but it should still be evaluated if it’s new or persistent.
Most early signs of breast cancer can also be caused by non-cancerous conditions like cysts or hormonal changes [cdc.gov]. However, any new breast change should be checked by a medical professional promptly. Early-stage breast cancer is often curable—but only if caught and treated early. Don’t wait or assume it will go away—it’s always better to get evaluated.
How to Perform a Breast Self-Exam (Step-by-Step)
Performing regular breast self-exams (BSE) is a simple, no-cost way to stay familiar with how your breasts normally look and feel [breastcancer.org]. This awareness helps you detect early signs of breast cancer or other unusual changes. In fact, about 1 in 4 breast cancer cases are first discovered by the patient through self-examination. While not a replacement for screenings like mammograms, self-exams are a valuable complement. Here’s how to perform one step-by-step:
- Choose a regular time: If you still have menstrual periods, the best time to examine your breasts is about a week after your period ends, when your breasts are least likely to be swollen or tender. If you no longer menstruate (post-menopausal), pick a consistent day each month (for example, the first of the month) to do your self-exam[my.clevelandclinic.org]. This routine helps you stay consistent..
- Visual inspection: Stand in front of a mirror with shoulders straight and hands on hips. Look for changes in size, shape, symmetry, dimpling, or nipple appearance. Raise your arms overhead and repeat the check. Then press your hands on your hips and flex your chest muscles to spot any subtle changes. Focus on noticing new or unusual differences. Note that it’s normal for the left and right breasts to not be perfectly symmetrical; focus on spotting new changes [myrtuemedical.org].
- Standing/pressing exam (in the shower): It’s easiest to feel for lumps when your skin is wet and slippery. Raise one arm behind your head. Using the pads of your three middle fingers (the flat part of the fingers, not the very tips), feel the entire breast and underarm in small circular motions—from collarbone to bra line and armpit to breastbone. Use light, medium, and firm pressure to detect any lumps or thickening [mayoclinic.org]. Gently squeeze the nipple to check for discharge. Repeat on the other side. This helps you catch early signs of breast cancer during routine self-checks.
- Lying down exam: Lie on your back with a pillow under your right shoulder and your right arm behind your head. Use your left hand to examine your right breast using small circular motions and varying pressure. Cover the entire breast and underarm area. Switch sides to check the left breast. Don’t forget to gently squeeze each nipple for discharge. This method helps detect early signs of breast cancer by flattening breast tissue for easier examination [nationalbreastcancer.org].
After completing the exam, take note of how your breasts normally feel. If you notice any new lump, hard knot, thickening, or other change, report it to your doctor. Most breast changes are not cancer, but it’s important to get them evaluated[my.clevelandclinic.org]. Performing self-exams monthly takes only a few minutes and can give you peace of mind – and if something is wrong, it could help catch it early.
Tip: You might find it helpful to use a diagram or illustration of the breast (divided into sections or a clock face) to ensure you systematically cover every part. There are many BSE guides and even wall charts available with step-by-step diagrams[amazon.com]. Familiarizing yourself with proper technique can improve the effectiveness of your self-exams.
Who Should Be Especially Vigilant? High-Risk Groups
While breast cancer can occur in any woman, certain individuals are at higher risk and should be extra vigilant about noticing early signs. High-risk groups include:
- Family history of breast or ovarian cancer: If your mother, sister, or daughter had breast cancer—especially at a young age—or there’s a family history of ovarian cancer, your risk is higher. Inherited gene mutations like BRCA1 or BRCA2 significantly increase the chance of developing breast cancer. About 5–10% of cases are linked to these mutations [cancer.org]. Women with a strong family history should talk to their doctor about genetic testing counseling and testing[cdc.gov] and may need earlier, more frequent screenings to catch the early signs of breast cancer than average-risk women[komen.org].
- Women with a personal history of breast conditions: If you’ve previously had breast cancer or certain benign breast conditions (such as atypical hyperplasia or lobular carcinoma in situ), your risk of developing breast cancer again is higher. These women should be very attentive to any new breast changes and follow their doctor’s recommendations for frequent check-ups.
- Younger women with dense breasts: Dense breast tissue increases the risk of breast cancer and makes detection harder on mammograms. Many younger women naturally have dense breasts. While screening often starts at age 40 in the U.S., about 10% of cases occur in women under 45 [acog.org].. In India, breast cancer is now the most common cancer among women, with a growing number of cases in women as young as their 30s. Indian women tend to be diagnosed at younger ages and at more advanced stages, partly due to lower awareness and limited access to screening. Whether in the U.S. or India, it’s crucial for younger women to stay breast-aware and recognize early signs of breast cancer, especially if they notice persistent or unusual changes [uclahealth.org].
- Women over 50: Age is the single most significant risk factor for breast cancer. The chance of developing breast cancer increases with each decade of life. Most breast cancers are diagnosed in women over 50 (the median age at diagnosis is 62)[cancer.umn.edu]. Women in their 50s and beyond should not only be breast-aware but also follow recommended screening guidelines (typically annual or biennial mammograms). Even if you’ve never had issues before, staying alert as you age is important.
- Men with risk factors: Although breast cancer in men is rare (accounting for about 1% of all breast cancers), men can and do develop breast cancer[cancercare.org]. Men with a strong family history of breast cancer or certain genetic mutations (like BRCA2) are at higher risk. Any lump or nipple discharge in a man should be checked by a doctor immediately.
If you’re in a high-risk group, speak with your doctor about a personalized screening plan. This may involve starting mammograms earlier, adding breast MRIs, or considering preventive options. Being high-risk doesn’t mean you’ll get cancer—but it does mean early detection is critical. Even if you’re at average risk, staying informed and breast-aware can help you recognize the early signs of breast cancer and act quickly if something changes. Knowing your body and family history is the first step in catching any potential problem early.
When to See a Doctor: Next Steps After Noticing Symptoms
If you detect a suspicious change in your breast – whether it’s a lump, skin change, nipple discharge, or anything else out of the ordinary – don’t panic, but do take action. Early breast cancer is often treatable, so prompt evaluation is key. Here’s what to do next:
- Make an appointment with your doctor: If you notice a breast change, contact your primary care physician or gynecologist promptly. Clearly describe the symptom—e.g., “a small lump in the upper outer area of my left breast, about the size of a pea.” Note when it appeared and any changes since. Early evaluation is key, especially since some appointments can happen within days. Men with breast symptoms should also seek prompt care, as male breast cancer is rare but often diagnosed late. Early signs of breast cancer should never be ignored—regardless of gender [cancer.org].
- Clinical breast exam: At your appointment, the doctor will examine your breasts and underarms. They will feel for lumps or thickening and check the size, shape, and texture of your breasts and nipples. They may also examine the lymph nodes in your armpit, as enlarged nodes can be a sign of cancer spread. Be honest about your concerns – doctors are used to evaluating breast changes and would rather see you for a check than miss a cancer.
- Diagnostic tests: Depending on what is found, your doctor may order imaging tests. The standard tests for evaluating breast symptoms are:
- Mammogram: An X-ray of the breast. If you’re over 40, you may already have had screening mammograms; in this case, the doctor will likely order a diagnostic mammogram (more detailed views of the area of concern). Mammograms can often detect tumors before they can be felt, so they are very useful for confirming or clarifying a lump[nationalbreastcancer.org].

Patient undergoing mammogram with medical professional adjusting equipment
- Ultrasound: A breast ultrasound uses sound waves to produce images of breast tissue. It’s often done along with a mammogram, especially if you’re younger or if the lump is near the surface. Ultrasound can help determine if a lump is a fluid-filled cyst (usually benign) or a solid mass. It’s painless and can be done right in the doctor’s office or imaging center.
- Biopsy: If imaging or a physical exam reveals a suspicious area, a biopsy is usually the next step. It’s the only way to definitively diagnose breast cancer. Depending on your case, your doctor may recommend a fine-needle aspiration, core needle biopsy, or surgical biopsy. The tissue sample is sent to a lab, where a pathologist checks for cancer cells. Results typically take a few days. Stay calm—many biopsies reveal benign (non-cancerous) conditions, but it’s important for confirming or ruling out early signs of breast cancer.
- After the diagnosis: If the biopsy confirms breast cancer, your care team will determine the stage and type, then outline treatment options. Early-stage breast cancer, especially when caught before it spreads, usually has an excellent prognosis [nationalbreastcancer.org]. Treatment may include surgery (lumpectomy or mastectomy), and possibly radiation, chemotherapy, hormone therapy, or targeted therapy depending on the cancer type. If the biopsy is benign, your doctor will explain the cause—like a cyst or fibroadenoma—and advise on follow-up. Either way, you gain clarity and can take the next step confidently.
Remember: Finding a breast symptom is not a death sentence – most breast lumps are not cancer[my.clevelandclinic.org]. However, it is a call to action. By seeing a doctor promptly, you ensure that if it is cancer, you catch it at the earliest, most treatable stage. If it’s not cancer, you can get appropriate care for whatever the issue is and avoid unnecessary worry. Early detection saves lives, so never delay getting a professional opinion about a breast change.
Why Early Detection Matters: Survival Rates and Treatment Options
Detecting breast cancer early can make a tremendous difference in the outcome. The earlier breast cancer is caught, the higher the chances of survival and the more treatment options are available. Here’s why early detection is so important:
- Higher survival rates: The stage at which breast cancer is diagnosed greatly impacts survival. When found early (localized), the 5-year survival rate is 99% [nationalbreastcancer.org]. This drops to 86% for regional spread and just 30% for metastatic cases. These numbers highlight why recognizing the early signs of breast cancer and getting timely screening can truly be life-saving.
- More treatment choices: Detecting breast cancer early allows for less aggressive treatment. Small, localized tumors can often be treated with a lumpectomy and radiation, preserving the breast. In contrast, advanced cancers may require mastectomy and chemotherapy. Early-stage cancer may also avoid chemo if it’s hormone-receptor positive and low-risk. Spotting the early signs of breast cancer gives patients more options and a better chance of maintaining quality of life.
- Better quality of life: Treating breast cancer early usually means less extensive treatment. Small tumors can often be removed with minimal impact on the breast, and avoiding metastasis means avoiding the complications of cancer in other organs. Patients with early breast cancer typically have shorter recovery times and fewer long-term side effects from treatment. In short, early detection can mean a shorter, gentler treatment journey and a return to normal life sooner.
- Peace of mind and proactive care: Catching the early signs of breast cancer—whether they lead to a negative result or a treatable diagnosis—can greatly reduce anxiety. Early detection puts you in control, allowing prompt treatment and access to clinical trials. In contrast, a late diagnosis often brings more stress, limited options, and greater emotional burden.
In summary, early detection saves lives and improves quality of life. Regular self-exams, clinical check-ups, and screening tests (like mammograms) are your best tools for catching breast cancer in its early, curable stages. By knowing the early signs of breast cancer and acting on them, you give yourself the best possible chance of beating the disease. Remember, breast cancer is often a slow-growing disease – if you catch it early, modern medicine can usually stop it in its tracks.
🔍 Also read: 10 Early Signs of Heart Attack You Should Never Ignore — Just like detecting early signs of breast cancer, spotting the signs of a heart attack early can be life-saving.
Support and Resources for Those Affected
Learning about breast cancer symptoms and undergoing screening or diagnosis can be an emotional journey. It’s important to know that you are not alone. There are many resources available to support you, whether you’re a woman facing a new diagnosis, a survivor, or a caregiver:
- Patient Support Organizations: Groups like Susan G. Komen, the National Breast Cancer Foundation, and Breastcancer.org offer a wealth of information, support services, and community for those affected by breast cancer. They provide helplines staffed by oncology professionals, online support groups, and financial assistance programs for things like mammograms or treatment costs[breastcancer.org]. For example, Komen’s Breast Care Helpline (1-877 GO KOMEN) connects you with trained oncology social workers who can answer questions and help find local resources[komen.org]. These organizations also host events (like Race for the Cure or local support meetings) that can connect you with others who have similar experiences.
- Patient Support Organizations: In the U.S., trusted groups like Susan G. Komen (1-877-GO-KOMEN), National Breast Cancer Foundation, and Breastcancer.org offer free helplines, financial aid, and support groups. In India, resources include The Pink Initiative, Can Protect Foundation, Yes to Life, and Hitaishini, which provide local language education, screenings, and survivor support. These platforms connect patients with guidance, community, and care throughout their journey.
- Local Support Groups: Many hospitals and cancer centers offer in-person breast cancer support groups, where sharing experiences can provide comfort and strength. In the U.S., the American Cancer Society and National Breast Cancer Foundation list support groups by location. In India, platforms like The Pink Initiative and Yes to Life connect patients with survivor-led meetups and virtual communities. If local options aren’t available, online groups on Facebook and forums offer round-the-clock support.
- Mental Health Support: A cancer diagnosis—or even the fear of one—can cause anxiety, stress, or depression. Many cancer centers offer counseling through oncology social workers or psychologists. If not, ask your doctor for a referral. Support is also available for caregivers and family members who may need help coping.
- Educational Resources: Empower yourself with knowledge. Reliable sources like the American Cancer Society (ACS) and National Cancer Institute (NCI) have detailed guides on breast cancer symptoms, screening, diagnosis, and treatment. The ACS website offers free booklets and fact sheets that you can download or request by mail[cancer.org]. The NCI provides a Breast Cancer Risk Assessment Tool online to estimate your personal risk[bcrisktool.cancer.gov]. These resources can help you understand medical terms, make informed decisions, and feel more in control of your situation.
- Financial Assistance and Navigation Programs: If cost is a concern, know that there are programs to help. The National Breast and Cervical Cancer Early Detection Program (NBCCEDP) offers free or low-cost mammograms and diagnostic services to women who are uninsured or underinsured[nationalbreastcancer.org]. Many hospitals have patient navigators who can guide you through the healthcare system and help find resources for treatment costs, transportation to appointments, or lodging during treatment. Organizations like CancerCare and The Pink Fund provide financial aid for things like utilities, mortgage, or groceries during active treatment[breastcancer.org]. Don’t be shy about asking for help – these services exist to support you through this challenging time.
- Survivorship and Thrivorship Resources: After treatment, many survivors benefit from survivorship programs that focus on long-term health, managing late effects of treatment, and emotional well-being. There are also groups specifically for young survivors, metastatic breast cancer patients, and other subgroups. The American Cancer Society’s programs include rides to treatment, lodging at Hope Lodges, and the Reach To Recovery program where a trained breast cancer survivor visits new patients to offer support and information[cancer.org].
Remember, reaching out for support is a sign of strength, not weakness. Breast cancer can be overwhelming, but with the help of supportive communities and professionals, you can navigate the journey with more confidence and less stress. You don’t have to face this alone – lean on your friends, family, and the many resources available to you. The breast cancer community is incredibly resilient and caring; connecting with others who understand what you’re going through can make a world of difference.
Conclusion
Breast cancer may be common, but it’s also one of the most treatable cancers – especially when caught early. By familiarizing yourself with the early signs of breast cancer and practicing regular breast self-awareness, you become your own best advocate in the fight against breast cancer. A small lump or subtle skin change might be nothing to worry about, but it could also be the first clue that leads to a life-saving diagnosis. Early detection saves lives, and it starts with you.
Here are the key takeaways from this article:
- Know your body: Perform monthly breast self-exams and get to know how your breasts normally look and feel. This way, you’ll notice any changes right away[breastcancer.org].
- Recognize the warning signs: Be alert for new lumps, thickening, skin changes, nipple discharge or inversion, pain, or other unusual breast changes[cdc.gov]. Not all changes are cancer, but all should be checked by a doctor.
- Don’t ignore risk factors: If you’re in a high-risk group (family history, genetic mutation, etc.), talk to your doctor about starting screenings earlier or more frequently[cancer.org]. Even if you’re at average risk, begin regular mammograms as recommended (usually by age 40–45) and continue through menopause and beyond.
- Act quickly: If you find something concerning, see a healthcare provider promptly. Early-stage breast cancer has a 99% 5-year survival rate[nationalbreastcancer.org] – the sooner you get evaluated, the better your outcome is likely to be.
- Support is available: Whether you’re seeking information, emotional support, or help with practical matters, there are resources and communities ready to assist you. Never hesitate to reach out for help.
Your health is your greatest asset. A monthly self-exam can help detect the early signs of breast cancer and potentially save your life. Men—share this knowledge with the women in your life. Women—commit to regular self-checks and schedule that mammogram if it’s due. Early detection starts with awareness.
Let’s make breast health a priority and empower ourselves with knowledge. Together, we can ensure that more women hear the words “it’s early” when diagnosed – a phrase that brings hope and a high chance of recovery. Stay informed, stay vigilant, and remember: you have the power to catch breast cancer early.
Share this article with your social network, family, and friends to spread awareness about early breast cancer signs. Your sharing could encourage someone to get checked out, potentially saving a life. Also, we’d love to hear your thoughts or experiences – feel free to leave a comment below. And if you found this information helpful, consider subscribing to our newsletter for more health tips and updates. Here’s to your health and well-being!
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
GOOD ARTICAL