Introduction: A New Reality for a Younger Generation
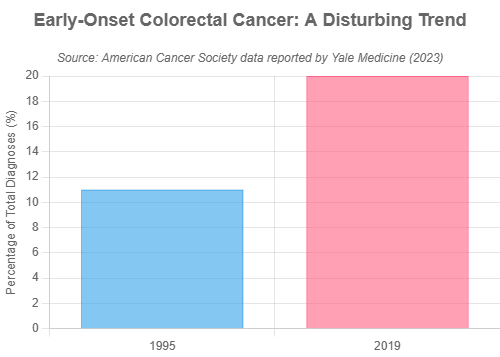
Colon cancer is no longer just a disease of the elderly. According to a 2024 report by the American Cancer Societ (ACS), it is now the leading cause of cancer-related deaths in men under 50 and the second in women. While overall colon cancer rates have declined due to screening in older adults, early-onset cases in people under 50 have nearly doubled since the 1990s. These younger cases are often diagnosed late because symptoms are overlooked or misdiagnosed.

A young adult patient in consultation with her doctor, a crucial step in addressing persistent health concerns.
This article is your essential guide to understanding the rise of colon cancer in young adults. You’ll learn the five key warning signs, explore the scientific reasons behind this trend—including lifestyle factors and gut health—and discover actionable steps to protect yourself. With real-life stories and clear screening guidelines, this post empowers you to take charge of your health and catch colon cancer early.
Table of Contents
The Core Issue: 5 Alarming Signs of Colon Cancer in Young Adults
While these symptoms don’t automatically mean colon cancer, persistence is the key warning sign. Many benign conditions can mimic them, but ongoing issues should not be ignored. The goal isn’t to cause panic, but to promote informed vigilance—so you know when to seek medical advice and rule out colon cancer early.
Key Insight from Research
A landmark study in the Journal of the National Cancer Institute found that young adults with just one symptom—like abdominal pain, rectal bleeding, diarrhea, or anemia—had nearly double the risk of a colon cancer diagnosis. Those with three or more signs faced a sixfold increase, highlighting how crucial these early warning symptoms are for detecting colon cancer.
1. Persistent Changes in Your Bowel Habits
A persistent change in your bowel habits—lasting weeks, not days—can be an early sign of colon cancer. It’s not just a reaction to food or stress, but a shift from your normal routine. Tumors in the colon may disrupt function, causing ongoing changes that shouldn’t be ignored.
- Diarrhea: More than just a single episode, this refers to frequent, loose, or watery stools that become a new pattern for you.
- Constipation: A new and persistent difficulty with bowel movements, involving straining, a feeling of blockage, or having significantly fewer movements than your norm.
- Narrow Stools: A distinct change in the shape or caliber of your stool, often described as becoming “pencil-thin.” This can be a physical sign that a tumor is partially obstructing the colon, forcing the stool to squeeze past it.
- Incomplete Evacuation: Medically known as tenesmus, this is a persistent sensation that you still need to have a bowel movement even after you’ve just been to the bathroom. It suggests something is irritating or blocking the rectum.
2. Rectal Bleeding or Blood in the Stool
A lasting change in bowel habits may signal colon cancer. It’s more than a reaction to food—persistent shifts from your norm shouldn’t be ignored.
The appearance can vary, providing clues about the location of the bleeding:
- Bright Red Blood: Often seen on toilet paper after wiping or as drops in the toilet bowl. This typically indicates bleeding in the lower part of the colon or the rectum.
- Dark, Tarry-Looking Stools (Melena): Stools that are black and sticky can be a sign of bleeding higher up in the digestive tract, as the blood has been digested.
- Blood Mixed with Stool: Stools that are streaked with or contain dark red blood can also signal a problem within the colon itself.
As Dr. Vikram Reddy, a Yale Medicine surgeon, emphasizes, “If anyone has any change in their bowel habits, if they have any bleeding—even if they think it’s a hemorrhoid, and it doesn’t go away—just get a colonoscopy.”
3. Unexplained Abdominal Pain, Cramps, or Gas
Persistent abdominal discomfort—not typical indigestion—can signal colon cancer. Tumors may block or irritate the colon, causing ongoing pain, gas, or bloating.

Persistent physical discomfort, such as abdominal or back pain, should not be dismissed, especially if it represents a new pattern.
Pay attention to these characteristics:
- A dull, persistent ache or pain in the abdomen that you can’t attribute to anything else.
- Frequent and severe gas pains or cramps that are out of the ordinary for you.
- A constant feeling of fullness or bloating that is new and doesn’t resolve with normal digestive processes.
The contextual clue is the change. If you’ve never been prone to such issues and they suddenly appear and persist, it’s a signal to seek medical advice.
4. Iron-Deficiency Anemia
This is a particularly stealthy but highly significant sign of colon cancer. A tumor in the colon can cause slow, chronic bleeding into the digestive tract. This blood loss is often invisible to the naked eye (occult blood), but over weeks and months, it can deplete the body’s iron stores, leading to an insufficient number of healthy red blood cells (anemia).

Unexplained and persistent fatigue, a potential sign of iron-deficiency anemia, can be a subtle but serious warning sign.
- Unusual Fatigue or Weakness: This is the hallmark symptom. It’s a profound sense of exhaustion that isn’t relieved by a good night’s sleep and a noticeable decrease in physical stamina.
- Pale Skin: A visible paleness in the skin, nail beds, and inside of the lower eyelids.
- Shortness of Breath: Feeling winded or out of breath from minor physical exertion, like climbing a single flight of stairs.
This sign is often discovered incidentally during a routine blood test, which highlights the immense value of regular health check-ups, even when you feel generally well.
5. Unexplained Weight Loss
Unexplained weight loss can be an early warning sign of colon cancer. Tumors may alter metabolism, suppress appetite, or drain the body’s energy—causing noticeable weight loss without lifestyle changes.
- What to Look For: A noticeable and unintentional drop in weight—for example, 5% or more of your body weight over a period of 6 to 12 months.
- A Combined Signal: This symptom becomes particularly concerning when it occurs in conjunction with any of the other four signs discussed above. For instance, unexplained weight loss combined with a change in bowel habits or anemia is a powerful signal that requires urgent medical evaluation.
The Science: Why Is This Happening to Younger People?
The rise in early-onset colon cancer has prompted global research into its causes. While genetics like Lynch syndrome explain some cases, most are linked to modern lifestyle factors and environmental exposures affecting younger generations.
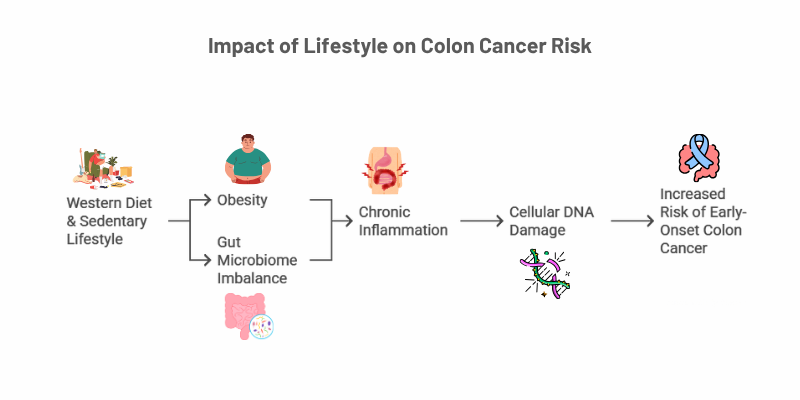
The “Western Lifestyle” Connection: Diet and Inactivity
The modern environment has been engineered for comfort and convenience, but this has come at a cost to our metabolic health. Several studies have identified a strong link between a “Western” lifestyle and increased cancer risk.
- Sedentary Behavior: especially prolonged sitting—has been linked to a higher risk of early-onset colon cancer. A study in JAMA Oncology found that extended TV time increased cancer risk, even among active individuals, due to harmful metabolic changes.
- Dietary Patterns: Diets high in red and processed meats, sugary drinks, and refined grains are strongly linked to colon cancer. Low fiber intake reduces protection and slows digestion, increasing the colon’s exposure to harmful substances.
- Obesity: Though not all young colon cancer patients are obese, excess body fat remains a key risk factor. Fat tissue produces hormones and inflammatory signals that can fuel cancer growth and chronic inflammation.

Diets high in processed foods, red meat, and sugar, characteristic of the “Western diet,” are strongly linked to an increased risk of colon cancer.
The Gut Microbiome’s Emerging Role
Your gut microbiome plays a vital role in health, and its imbalance—known as dysbiosis—may drive early-onset colon cancer. A 2025 NPR-highlighted study found that a toxin called colibactin, produced by certain E. coli strains, can damage colon cell DNA. This genotoxic signature was far more common in tumors from younger patients, linking microbial activity directly to cancer development.
“Just like microplastics can silently disrupt brain function, emerging research shows that gut imbalances and toxins may play a role in colon cancer. Learn how invisible threats like microplastics affect your body here.
Chronic Inflammation: The Silent Driver
Chronic inflammation is the hidden link between poor lifestyle, microbiome imbalance, and colon cancer. Unlike short-term inflammation from injury, this slow-burning, long-term process damages cells over time. It fuels cancer by causing DNA damage, speeding up cell turnover, and creating a growth-friendly environment for tumors—especially in the gut.
- DNA Damage: Inflammatory processes release reactive oxygen species (free radicals) that can directly damage the DNA of colon cells, leading to mutations.
- Accelerated Cell Turnover: To repair the damage from inflammation, the body increases the rate at which colon cells divide and are replaced. This rapid division increases the chances of errors (mutations) occurring and being passed on.
- Pro-Growth Environment: Chronic inflammation creates a microenvironment rich in growth factors and signaling molecules that can help nascent cancer cells survive, proliferate, and form a tumor. It’s akin to providing the perfect, fertile soil for a dangerous seed to grow.
Real Stories, Real Stakes: Voices of Young Survivors
Statistics provide the scale of the problem, but personal experiences reveal its human cost and underscore the critical importance of self-advocacy. The stories of young people who have faced this diagnosis are powerful testaments to the need for vigilance.
Savannah’s Story: Pushing for Answers
At just 26, Savannah Kaspar experienced abdominal pain and bloody stools. Initially dismissed as hemorrhoids or IBD, her symptoms were overlooked due to her age. Trusting her instincts, she insisted on a colonoscopy—revealing a colon cancer diagnosis. Her determination led to early detection that may have saved her life. Her Detailed story is shared by MD Anderson Cancer Center.
The Lesson: You are the world’s foremost expert on your own body. If something feels persistently wrong, do not be dismissed. Insist on a thorough investigation until you have clear answers.
Ben’s Story: Listening to Your Body
Ben Simcox’s journey, chronicled by the Cleveland Clinic, with a family history of colon cancer, had a clear screening at 28. Years later, as a young father, he noticed bowel changes and blood in his stool. Recognizing the risks, he acted quickly and was diagnosed with rectal cancer—caught early enough to treat. His swift response likely saved his life.
The Lesson: Do not delay. Embarrassment or fear can be formidable barriers, but a day of discomfort for a screening procedure is infinitely preferable to a late-stage cancer diagnosis that limits your options.
The Screening Dilemma: A Balanced View for Young Adults
With early-onset colon cancer on the rise, health authorities have lowered the recommended screening age. Now more than ever, knowing when to screen and which method to choose is vital. Understanding your options helps you make informed, personalized decisions with your doctor.
| Aspect | The Benefits (Pros) | The Challenges (Cons) |
|---|---|---|
| Early Screening (e.g., Colonoscopy) | Can find and remove precancerous polyps, preventing cancer from ever developing. It is both a diagnostic and preventative tool. | It is an invasive procedure that requires sedation and carries small but real risks, such as bleeding or perforation of the colon. |
| Dramatically increases survival rates. When caught at a localized stage, the five-year survival rate is over 90%. | Cost, insurance coverage, and accessibility can be significant barriers, especially for younger or uninsured individuals. | |
| Stool-Based Tests (e.g., FIT, Cologuard) | Non-invasive, can be done in the privacy of your home, and are generally more affordable and accessible. | They are less sensitive than a colonoscopy and can produce false positives (causing anxiety and unnecessary follow-up) or false negatives (missing a cancer). |
| Their convenience can increase overall participation in screening programs, catching more cancers in the population. | A positive result is not a diagnosis. It must be followed by a diagnostic colonoscopy to determine the cause. |
Know the Official Guidelines
The guidelines provide a clear starting point for conversations with your doctor:
- Average Risk: Both the American Cancer Society (ACS) and the U.S. Preventive Services Task Force (USPSTF) recommend that individuals at average risk begin regular screening at age 45.
- High Risk: You are considered high-risk and should discuss starting screening earlier than age 45 with your doctor if you have any of the following:
- A personal history of colorectal cancer or certain types of polyps.
- A strong family history of colorectal cancer or polyps (e.g., a first-degree relative diagnosed before age 60).
- A personal history of inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis.
- A known or suspected genetic syndrome, such as Lynch syndrome or Familial Adenomatous Polyposis (FAP).
- A personal history of colorectal cancer or certain types of polyps.
Common Questions & FAQs
If I have one of these symptoms, does it automatically mean I have colon cancer?
Absolutely not. It’s important to reiterate that these symptoms are common and can be caused by a wide range of conditions, including Irritable Bowel Syndrome (IBS), IBD, infections, or hemorrhoids. However, you cannot and should not self-diagnose. The only way to determine the cause is to see a doctor for a proper evaluation. The key takeaway is not to panic, but also not to ignore persistent symptoms that represent a change for your body.
I’m young, fit, and eat a healthy diet. Why should I be concerned about this?
This is a crucial and common misconception. While a healthy lifestyle significantly reduces your risk, it does not eliminate it entirely. As noted by clinicians at the American College of Surgeons, a perplexing aspect of this trend is the increasing number of young, fit patients with no traditional risk factors who are being diagnosed. The rising incidence is a population-level phenomenon, making awareness of the warning signs essential for everyone, regardless of their fitness level.
What is the first step if I’m worried about a symptom?
The first and most important step is to schedule an appointment with your primary care physician or a gastroenterologist. Prepare for your appointment by writing down your symptoms, when they started, how frequent they are, and any other relevant details. Be direct, specific, and honest. Do not let embarrassment about discussing bowel habits prevent you from having a conversation that could potentially save your life.
Conclusion: Your Health Is in Your Hands—Take Action Now
Colon cancer is no longer limited to older adults—its sharp rise in young people is a wake-up call. Recognizing five key warning signs—bowel changes, rectal bleeding, abdominal pain, anemia, and weight loss—is crucial for early detection. Awareness turns you from a passive observer into an empowered advocate for your own health.
Your Action Checklist
- Listen to Your Body: Begin today to pay close, non-anxious attention to your body’s normal rhythms and signals. Acknowledge what is normal for you so you can recognize what is not. Don’t brush off persistent changes as “just stress” or “something I ate.”
- Advocate for Your Health: If you experience any of the five signs for more than a couple of weeks, make a doctor’s appointment. Go into that appointment prepared to be your own best advocate. Clearly state your symptoms and your concerns about the rising rates of early-onset colon cancer.
- Know Your Family History: Have explicit conversations with your relatives. Ask if anyone in your family has had colorectal cancer or polyps. Understanding your family’s health history is a critical piece of your personal risk assessment and will inform your doctor’s recommendations.
- Adopt a Proactive Lifestyle: You can take concrete steps to lower your risk. Focus on reducing your intake of red and processed meats, increasing your fiber intake through a diverse range of fruits and vegetables, and making regular physical activity a non-negotiable part of your daily routine.
Have you or someone you know been affected by early-onset colorectal cancer? Sharing your experience in the comments can help raise awareness and reduce the stigma. Please forward this article to the young people in your life—your friends, your children, your colleagues. It’s a simple act that could save a life.
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.