Introduction: A New Reality for Medical Education
Imagine a surgical resident in a remote clinic, moments before a complex cardiac operation. She slips on a lightweight headset and enters a virtual operating room—complete with a 3D replica of her patient’s heart built from MRI and CT scans. Guided in real time by a specialist across the globe, she practices every incision and refines her technique with precision.
This isn’t science fiction—it’s the new era of AR/VR in Medical Training, transforming how healthcare professionals learn, rehearse, and perform. The traditional “see one, do one, teach one” model is evolving as immersive simulations deliver safer, faster, and more standardized learning experiences.
The momentum is undeniable: the global AR/VR healthcare market, valued at $3.9 billion in 2024, is expected to soar beyond $30 billion by 2034. This guide explores the best AR and VR tools for medical education in 2025, real-world use cases, and how immersive technology is reshaping the future of clinical training.
Table of Contents
Why AR/VR is Revolutionizing Medical Training
The transition towards immersive technologies is not just about adopting novel gadgets; it’s about fundamentally solving the core limitations of traditional medical education. By creating controlled, repeatable, and data-rich learning environments, AR/VR addresses long-standing challenges related to risk, accessibility, and standardization.
Problem: High-Risk, High-Stakes Initial Practice
The “do one” phase of traditional training often means a trainee’s first attempt at a procedure is on a live patient. While supervised, this carries inherent risks and immense pressure. Cadavers are a limited and expensive resource, and animal labs present ethical and anatomical discrepancies.
Solution: Immersive, Risk-Free Simulation.
VR platforms create hyper-realistic, repeatable clinical environments—from operating rooms to emergency bays—where trainees can practice high-stakes procedures without any patient risk. Whether it’s laparoscopic surgery or crisis response, learners can repeat scenarios until they build true muscle memory, procedural fluency, and confident decision-making.Platforms like Osso VR allow complete control of the virtual environment, letting trainees rotate, zoom, and interact from any angle—far beyond the limits of traditional 2D training.
Problem: Inconsistent and Geographically Limited Training
The quality of an apprenticeship can vary significantly based on the instructor’s teaching style, the caseload at a particular hospital, and the trainee’s geographic location. A student in a rural area may never get exposure to the complex cases seen at a major urban medical center, creating a gap in expertise.
Solution: Standardized and Scalable Learning.
AR/VR in Medical Training delivers a consistent, high-quality curriculum to learners anywhere in the world. A Texas Tech case study showed how VR successfully trained physician assistant students in remote rural settings, bridging geographic gaps and enabling interprofessional learning that traditional methods cannot offer. This democratization of expertise ensures uniform training standards and helps reduce workforce shortages in underserved regions.
Problem: Subjective and Delayed Feedback
Assessing a trainee’s performance has historically relied on the subjective observation of a supervising physician. Feedback can be inconsistent, delayed, and may not capture the fine details of a trainee’s technique or decision-making process.
Solution: Data-Driven, Objective Assessment.
Modern AR/VR in Medical Training systems act as powerful data engines, tracking every movement, decision, and error with millimetric accuracy. A BMC Surgery review showed that metrics such as task time, instrument path length, and error rates provide far more objective feedback than traditional observation. This detailed, quantifiable assessment enables targeted coaching and a clearer, evidence-based measure of clinical competency.
As AR/VR in medical training reshapes how future clinicians learn, it also fits into the broader set of high-impact healthcare tech skills professionals must master in 2025—a trend that every medical learner should stay ahead of.
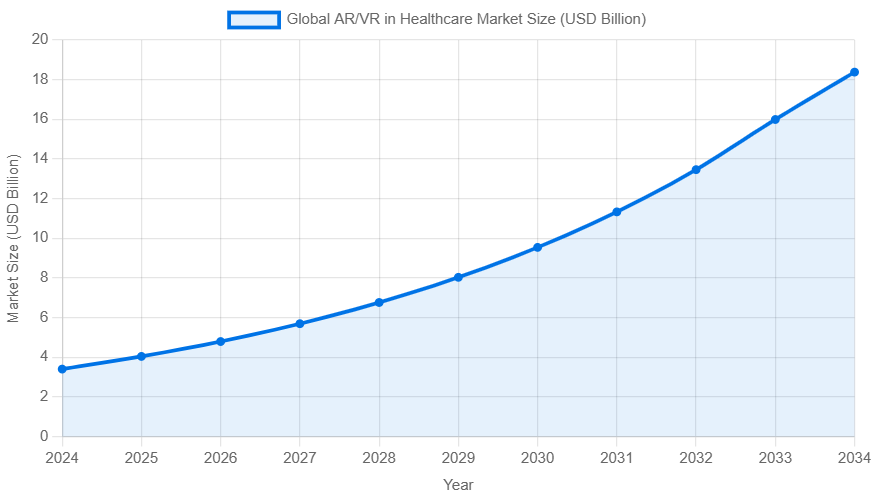
Projected growth of the global AR/VR in healthcare market, demonstrating rapid adoption. Data source: Precedence Research.
Core Applications of AR/VR in Medical Training
The application of immersive technology in medicine is broad and expanding rapidly. By breaking down the primary use cases, we can see how AR/VR is tailored to meet the specific needs of different medical disciplines and learner profiles, from first-year medical students to experienced surgeons.
Surgical Simulation: Rehearsing for Perfection
Target Audience: Surgeons, Residents, Medical Institutions
Surgical simulation is arguably the most mature and impactful application of VR in healthcare. It transforms the operating room from a place of first-time performance into a stage for rehearsed excellence. The goal is simple and profound: as surgical simulator company VirtaMed puts it, to ensure surgeons “never perform a procedure for the first time on a patient.”

Procedural Mastery
VR simulators enable deliberate, repeatable practice of complex surgeries across multiple specialties. Platforms such as VirtaMed offer modules like ArthroS™ for orthopedic procedures, LaparoS™ for laparoscopic training, and RoboS™ for robotic surgery. Many systems also include haptic feedback, mimicking real tissue resistance and instrument feel—an essential realism that traditional training methods cannot match.
Pre-Operative Planning
Beyond general skill training, AR/VR in Medical Training enables true patient-specific rehearsal. Surgeons can convert a patient’s CT and MRI scans into interactive 3D VR models, allowing them to “walk through” the unique anatomy before surgery. This helps plan the safest approach, anticipate challenges like atypical vasculature or tumor location, choose the right instruments, and ultimately reduce operating time while improving surgical precision.
Proven Outcomes
The benefits of AR/VR in Medical Training are strongly supported by evidence. A 2024 BMC systematic review found that VR-trained surgeons consistently show faster task completion, smoother instrument handling, greater movement efficiency, and fewer intraoperative errors. These results confirm that VR simulators enhance surgical skills at every experience level, leading to better comprehension, confidence, and overall performance.
Anatomy Education: Bringing the Human Body to Life
Target Audience: Medical Students, Educators
For generations, medical students have learned anatomy from dense textbooks, 2D diagrams, and the limited, non-repeatable experience of cadaver dissection. AR and VR are shattering these limitations, offering dynamic, interactive, and deeply intuitive ways to understand the complex architecture of the human body.

Beyond the Textbook
With AR/VR in Medical Training, students no longer rely on static images. They can virtually dissect a 3D body, isolate entire systems, peel back muscle layers, and explore anatomical structures from any angle. This hands-on, exploratory learning dramatically improves spatial understanding and retention. Platforms like Complete Anatomy, inspired by Gray’s Anatomy, offer a cutting-edge 3D environment for immersive anatomy education.
The Power of Augmented Reality
AR takes AR/VR in Medical Training even further by overlaying digital anatomy onto the real world. With a tablet or AR glasses, students can project a full-scale virtual human body into their study space, walk around it, and examine structures from every angle. Apps like AR Anatomy and VOKA 3D Anatomy make learning more interactive and effective by connecting abstract concepts with a realistic 3D view of the body.
Key Platforms for 2025
The market for anatomy apps is rich and competitive. Leading platforms for 2025 include:
- Complete Anatomy: Known for its incredibly detailed 3D models, extensive library of videos, and virtual dissection capabilities.
- Human Anatomy Atlas 2026: Offers robust male and female models, a video library for patient education, and specialized dental anatomy modules.
- VOKA 3D Anatomy & Pathology: Uniquely integrates normal anatomy with gross pathology in 3D, allowing students to compare healthy and diseased states side-by-side.
Nursing and Procedural Training: Enhancing Clinical Skills
Target Audience: Nurses, Nursing Students, Allied Health Professionals
The scope of AR/VR training extends far beyond the operating room and anatomy lab. It is becoming an indispensable tool for nurses and other healthcare professionals, providing a safe space to develop both hard clinical skills and crucial soft skills.

Crisis and Emergency Response
Nurses are often the first responders in unpredictable, high-pressure situations. With AR/VR in Medical Training, they can safely experience rare but critical events—such as mass-casualty incidents, infectious disease outbreaks, or cardiac arrest scenarios. As noted by ScienceSoft, these immersive crisis simulations help nurses build automatic response patterns, sharpen critical thinking, and perform more confidently under extreme stress.
Procedural Competency and Soft Skills
VR offers a safe, controlled environment for nurses to practice delicate procedures such as IV insertion, wound care, and operating complex equipment. Beyond technical skills, AR/VR in Medical Training is increasingly used to build soft skills—like patient communication, empathy, and managing difficult conversations. Platforms such as SimX even support multiplayer scenarios, allowing nurses, physicians, and first responders to train together and strengthen teamwork and communication during virtual emergencies.
The Tech Toolkit: Top Platforms and Tools for 2025
Choosing the right AR/VR solution depends heavily on the specific training goal, target user, and budget. The market offers a spectrum of options, from comprehensive surgical simulators with haptic feedback to accessible mobile apps for anatomy education. Below is a comparative overview of some of the leading platforms shaping medical training in 2025.
| Tool/Platform | Primary Technology | Key Features & Modules | Typical Application | Target Users |
|---|---|---|---|---|
| Osso VR | VR | Surgical procedure simulation, collaborative multiplayer training, performance analytics, objective assessment. | Orthopedic and other surgical skill training, medical device training. | Surgeons, Residents, Medical Device Companies |
| VirtaMed | Mixed Reality/VR | High-fidelity haptic feedback, realistic physical anatomical models blended with VR graphics. | Orthopedics (ArthroS™), OB/GYN (GynoS™), Urology (UroS™), Laparoscopy (LaparoS™). | Surgeons, Hospitals, Training Institutions |
| SimX | VR | Multiplayer scenarios, customizable patient cases with evolving vitals, AI-powered virtual patients. | Emergency response, team-based crisis training, clinical case practice. | First Responders, Nurses, Physicians, PAs |
| Complete Anatomy | AR/3D | Detailed 3D human atlas, virtual dissection, animations of muscle movement, quizzes, AR mode. | Anatomy education, patient communication, student self-study. | Medical Students, Educators, Clinicians |
| HoloPatient (by GIGXR) | AR/Mixed Reality | Holographic standardized patients that can be placed in a real environment, remote learning capabilities. | Clinical assessment, nursing skills training, patient interaction practice. | Medical & Nursing Schools, Institutions |
The Next Frontier: Digital Twins in Surgical Planning
While VR simulation offers powerful training on generic or case-specific models, the ultimate frontier in personalized medicine is the “;digital twin.” This concept, targeting the most innovative and forward-looking segments of healthcare, represents a paradigm shift from reactive treatment to proactive, predictive, and hyper-personalized intervention.
What is a Digital Twin?
A digital twin is much more than a static 3D model—it’s a dynamic, virtual replica of a patient that updates continuously with real-time clinical data. Information from EHRs, lab results, genetic profiles, and wearable sensors feeds this evolving “patient-in-silico,” mirroring the person’s health status over time. In the context of AR/VR in Medical Training, digital twins offer a powerful, personalized view of patient anatomy and physiology, enabling deeper understanding and more precise clinical planning.

Application in Personalized Surgery
In surgery, digital twins take AR/VR in Medical Training to the next level by allowing clinicians to rehearse personalized procedures on a virtual replica of the actual patient. Researchers at Duke University’s Center for Computational Health show how surgeons can use a vascular digital twin to test different stent sizes and placements to predict the best blood-flow outcome—all before making a single incision. This empowers surgeons to:
- Simulate surgical outcomes: Test different techniques to predict which will be most effective for that patient’s unique physiology.
- Predict and prevent complications: Identify potential risks based on the dynamic model’s response to simulated interventions.
- Optimize procedures: Refine the surgical plan for maximum efficacy and minimum risk, truly personalizing the care delivered .
While still largely in the experimental phase, digital twin-assisted surgery holds the promise of making procedures safer, more effective, and tailored to the individual like never before.
Weighing the Options: Benefits and Challenges of AR/VR Adoption
Like any transformative technology, the integration of AR/VR into medical training presents both immense opportunities and significant hurdles. A balanced, realistic perspective is crucial for any institution or individual considering adoption.
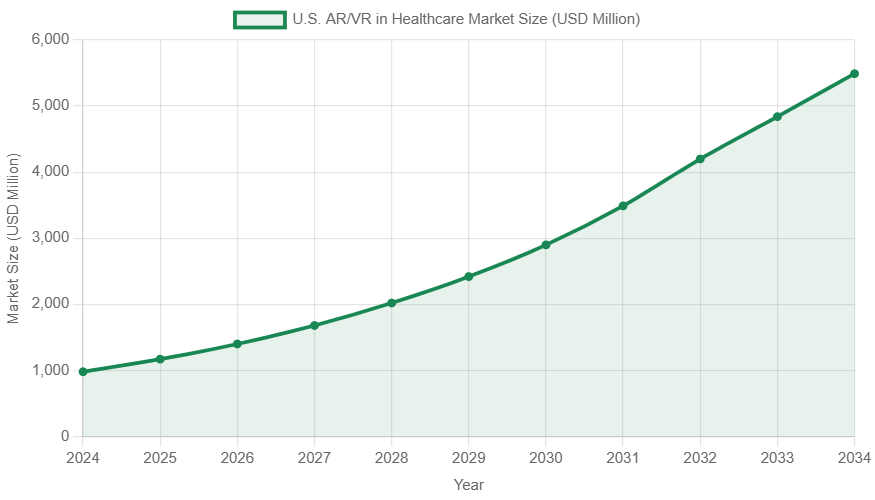
The U.S. market shows strong, consistent growth, reflecting high demand and investment. Data source: Precedence Research.
The Advantages (Pros)
- Improved Learning Outcomes & Retention: Immersive, hands-on learning is fundamentally more effective than passive observation. A study with the University of Plymouth showed that medical students demonstrated significantly higher levels of accuracy in equipment knowledge after VR training compared to before .
- Significant Cost Reduction Over Time: Although the upfront investment can be high, AR/VR in Medical Training delivers a strong long-term ROI. It reduces or eliminates recurring expenses for cadavers, animal labs, and costly physical mannequins. One analysis showed that replacing mannequin-based training with VR for pulmonary disease education resulted in a 3× cost reduction while maintaining excellent performance outcomes.
- Enhanced Patient Safety: This is the ultimate and most important benefit. Better-trained, more confident clinicians make fewer mistakes. By allowing trainees to master procedures in a zero-risk environment, AR/VR directly contributes to improved patient outcomes and reduced complication rates.
- Democratized Access to Expertise: AR/VR technology breaks down geographical barriers, allowing world-class training and expert mentorship to reach professionals in remote or underserved areas. This is critical for addressing global health disparities and standardizing care quality .
The Hurdles (Cons)
- High Initial Investment: The upfront cost remains a significant barrier. A full-fledged, custom medical training VR application can range from $120,000 to $360,000, in addition to hardware costs for headsets and powerful PCs .
- Lack of Haptic Realism: While improving, haptic feedback technology still struggles to perfectly replicate the nuanced feel of living tissue, the tension of a suture, or the vibration of a surgical drill. For procedures that rely heavily on the sense of touch, this remains a key limitation .
- Content Standardization and Validation: The market is fragmented, with many proprietary systems. There is a pressing need for more clinically validated, peer-reviewed training modules that are recognized by accrediting bodies and can be integrated into official curricula. Without this, it’s difficult for institutions to ensure quality and consistency .
- Integration and Usability Issues: Technical challenges persist, including difficulties integrating VR training platforms with existing hospital IT systems like EHRs. On the user side, issues like cybersickness (VR-induced motion sickness), the physical weight of headsets, and the “cognitive load” of navigating complex virtual interfaces can hinder adoption.
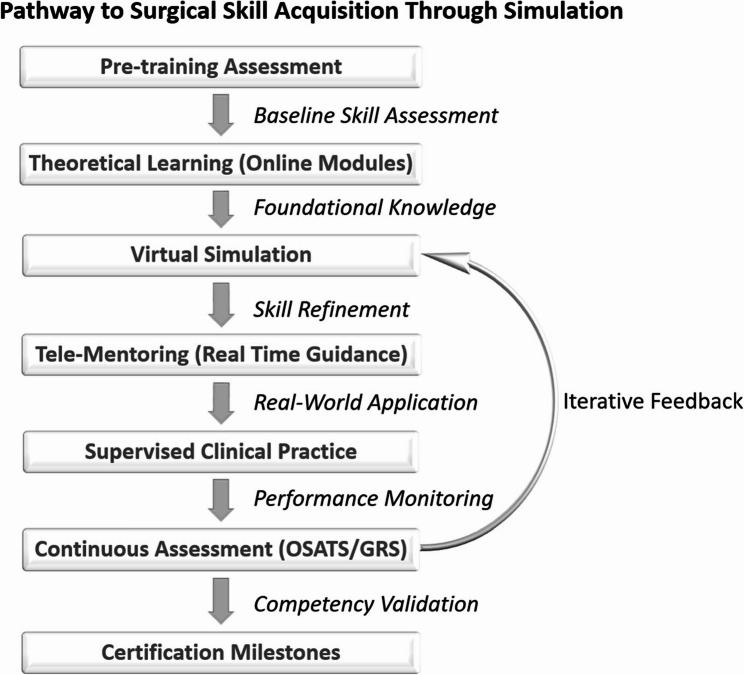
Getting Started: A Strategic Roadmap for Implementation
For medical schools, hospitals, and training institutions, the question is no longer *if* they should adopt AR/VR, but *how*. A strategic, phased approach is key to a successful implementation that maximizes ROI and minimizes disruption.
- Start with a Needs Assessment: Before adopting AR/VR in Medical Training, identify the most important training gaps in your institution. Is there a high-risk, low-frequency procedure trainees struggle with? Limited access to anatomy labs? Or a need to improve team communication during emergencies? Defining a clear problem statement ensures the technology is implemented with purpose and delivers maximum impact.
- Form a Multidisciplinary Team: Successful implementation requires buy-in from all stakeholders. Form a team that includes clinicians and educators who will use the technology, IT staff who will support it, administrators who will fund it, and students or residents who will be the end-users.
- Launch a Focused Pilot Program: Avoid a large-scale, institution-wide rollout at first. Start small and focused. For example, pilot a platform like Osso VR for a single orthopedic procedure in one residency program, or use an app like Complete Anatomy to supplement one module of the first-year anatomy course. This allows you to learn and adapt in a low-risk setting.
- Measure, Evaluate, and Report: Before the pilot begins, define clear success metrics. These should be a mix of quantitative data (e.g., assessment scores from the simulator, reduction in training time, user engagement rates) and qualitative feedback (e.g., surveys on user confidence, perceived realism, and usability).
- Iterate and Scale: Use the data and feedback from your pilot program to build a strong business case for expansion. The results can justify a wider rollout, help refine the training protocols, and secure funding for further investment. This iterative process ensures that the program grows based on proven value.
Frequently Asked Questions (FAQs)
Q1: What is the typical budget for a basic VR training setup?
A: The cost varies widely. A starter setup for an individual or small group can range from a few thousand dollars, covering consumer-grade headsets (like the Meta Quest 3) and off-the-shelf software licenses (e.g., a subscription to Complete Anatomy). At the other end, a single high-fidelity surgical simulator with proprietary hardware and haptics can exceed $50,000. As noted by ScienceSoft, a full institutional program with custom content can range from $120,000 to over $360,000, depending on scale and complexity.
Q2: Should we invest in AR or VR for medical training?
A: This is not an either/or choice; it’s about selecting the right tool for the job.
Virtual Reality (VR) is ideal for fully immersive simulations where the user needs to be isolated from the real world to focus on a complex virtual task (e.g., performing a complete surgery in a simulated OR).
Augmented Reality (AR) excels when digital information needs to be overlaid onto the real world or a physical mannequin (e.g., projecting vein anatomy onto a patient’s arm for IV placement practice or providing real-time guidance during a procedure).
The future likely lies in Mixed Reality (MR), which seamlessly blends the real and virtual worlds, offering the benefits of both.
Q3: How can we measure the Return on Investment (ROI) of AR/VR training?
A: ROI should be measured holistically, considering a combination of factors:
Direct Cost Savings: Reduced spending on cadavers, animal labs, disposable supplies, and travel for specialized training.
Efficiency Gains: Measurable reductions in operating room time for trained surgeons, faster onboarding of new staff, and shorter overall training times to reach proficiency.
Improved Clinical Outcomes: The most valuable, though hardest to quantify, return. This includes lower complication rates, fewer medical errors, and better patient safety metrics, which ultimately reduce long-term healthcare costs associated with adverse events.
Enhanced Competency & Confidence: Higher scores on standardized assessments (like the Objective Structured Assessment of Technical Skills – OSATS) and increased trainee confidence, which correlates with better performance.
Conclusion: The Future of Training is Immersive
In 2025, AR/VR in Medical Training is no longer a novelty—it has become a core pillar of high-quality, efficient, and safe medical education. From the anatomy lab to the operating room, immersive technologies are solving long-standing training challenges and preparing the next generation of clinicians for the demands of modern healthcare.
The evidence is undeniable: AR/VR improves learning, lowers costs, and significantly enhances patient safety. The question for healthcare institutions and educators is no longer whether to adopt this technology, but how to integrate it strategically to gain a competitive edge, expand access to expertise, and elevate the standard of care for every learner and patient.
