Introduction: From Burnout to Breakthrough
For many clinicians, the workday extends into “pajama time”—evening hours spent catching up on EHR tasks. Studies show that 34% to 55% of their day goes to documentation, fueling burnout and reducing patient interaction. AI for clinical documentation offers a powerful solution to this growing crisis.
But a technological shift is underway. AI for clinical documentation is no longer a futuristic concept but a practical, powerful solution being deployed in health systems today. It promises to automate tedious tasks, restore the human connection in medicine, and give clinicians back their time. This article provides a comprehensive guide to this transformation, exploring:
- The core AI technologies revolutionizing documentation.
- A review of the leading tools and platforms available in 2025.
- A practical framework for integrating these tools into clinical workflows.
- Real-world case studies demonstrating proven return on investment (ROI).
- A balanced look at the implementation challenges and the future of AI in healthcare.
Table of Contents
Why AI? The Driving Force Behind the Documentation Revolution
The “clerical burden” in healthcare is a systemic issue that drains time from patient care and fuels clinician burnout. Every moment spent typing is one lost in connection and diagnosis. AI for clinical documentation addresses this challenge by streamlining how medical data is captured, allowing clinicians to focus on care, not clicks.
The Technology Explained
Three key AI technologies form the backbone of this documentation revolution:
- Natural Language Processing (NLP) is the core of AI for clinical documentation. It enables computers to understand and analyze physician-patient conversations and unstructured notes, extracting key medical details like symptoms, diagnoses, and treatment plans. NLP is a leading trend driving faster, Its use is a key trend for more accurate clinical documentation.
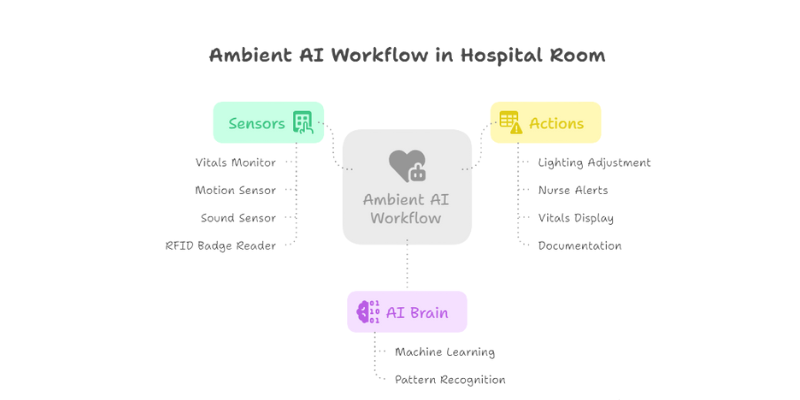
- Ambient Clinical Intelligence: Ambient AI acts like an invisible medical scribe—capturing clinician-patient conversations in real time. Using discreet microphones, it records and processes dialogue without requiring any manual input, allowing physicians to stay fully engaged. As part of AI for clinical documentation, this technology reduces screen time and enhances patient interaction.
- Generative AI: Generative AI builds on NLP by transforming transcribed conversations into structured clinical notes—often formatted into SOAP (Subjective, Objective, Assessment, Plan) sections. Powered by large language models like those behind ChatGPT, it enables fast, accurate documentation. Tools like Abridge use generative AI , making AI for clinical documentation smarter and more efficient than ever.
The Modern Clinician’s Toolkit: Top AI Tools for Clinical Documentation
The market for AI for clinical documentation is growing fast. Most tools fall into two main categories: ambient AI scribes that capture the full patient encounter, and specialized tools that streamline specific steps in the documentation workflow.
Ambient AI Scribes: Your Behind-the-Scenes Documentation Partner
These platforms are designed to be all-in-one solutions that record, transcribe, and summarize patient encounters into draft clinical notes, which the clinician then reviews and finalizes. They represent the most significant shift in clinical workflows.
- Abridge: A leader in the space, Abridge is used by major health systems like the University of Chicago Medicine. Its platform is trained across over 50 specialties and supports more than 28 languages. It’s known for deep EHR integration, especially with Epic, allowing for a seamless workflow.
- DeepScribe: This platform focuses on real-time, AI-powered transcription and note generation. DeepScribe aims to free clinicians from the keyboard by automatically creating notes from patient interactions, integrating directly with EHRs to enhance efficiency.
- ScribeHealth: Positioning itself as a powerful alternative, ScribeHealth emphasizes the automation of SOAP notes and integrated medical coding. It claims to reduce charting time by up to 70%, a significant productivity gain for busy practices.
- Augmedix: Specializing in ambient medical documentation, Augmedix provides technology that converts natural clinician-patient conversations into real-time medical records, aiming to streamline workflows and reduce the manual effort of documentation.
Beyond Transcription: AI for Data Structuring and Medical Coding
Beyond creating notes from conversations, AI is also being used to analyze existing unstructured text within the EHR to perform highly valuable, specific tasks.
- Automated Medical Coding: AI tools can scan clinical notes to identify relevant diagnoses and procedures, suggesting the appropriate ICD-10 and CPT codes. This not only speeds up the billing cycle but also improves coding accuracy, reducing claim denials and preventing revenue leakage.
- Data Structuring: A significant portion of clinical data is locked away in narrative text. AI can extract this information—such as lab values, medication mentions, or social determinants of health—and convert it into structured data fields. This makes the data queryable for clinical research, population health initiatives, and quality reporting.
- Quality Evaluation: According to a systematic review, AI tools are being developed to evaluate documentation quality by auditing notes for completeness, consistency, and compliance with regulatory or institutional guidelines.
The “How-To”: Integrating AI into Your Clinical Workflow
Adopting AI for clinical documentation is more than a technology purchase; it’s a strategic change management process. Successful implementation hinges on thoughtful planning and a focus on integrating the tool seamlessly into existing clinical workflows.
A 4-Step Framework for Successful Implementation
- Assess & Plan: Start by identifying your biggest documentation challenges—whether in primary care, emergency medicine, or a surgical specialty. Set clear goals for implementing AI for clinical documentation, like reducing note completion time by 50% or eliminating after-hours charting within three months.
- Select the Right Vendor: Move beyond marketing claims and conduct rigorous due diligence. A best practice is to follow the model used by institutions like the Cleveland Clinic, which ran a head-to-head pilot of multiple vendors. Key evaluation criteria should include: clinical accuracy, ease of use for providers, depth of EHR integration, robust security and HIPAA compliance, and a clear, demonstrable ROI.
- Pilot & Train: Start small. Roll out the chosen tool to a limited group of enthusiastic early adopters. This pilot phase is crucial for gathering feedback on workflow friction and building momentum. Provide comprehensive training and identify “super-users” who can act as internal champions and support their peers.
- Scale & Optimize: Based on the success and learnings from the pilot, develop a phased rollout plan for the broader organization. Continuously monitor key performance indicators—time saved, coding accuracy, user satisfaction surveys, and patient feedback—to fine-tune the implementation and maximize value.
The New Workflow in Action: A Before-and-After Scenario
Before AI: The clinician sits across from the patient, their attention divided between the conversation and the computer screen. They type frantically to capture key details, often interrupting the flow of the visit. Documentation is frequently incomplete and must be finished hours later, at home.
With Ambient AI: The workflow is transformed into a more natural, human-centered experience.
- Step 1: Obtain Consent. The clinician begins the visit by informing the patient about the AI scribe and obtaining their verbal consent to record the conversation.
- Step 2: Focus on the Patient. The clinician puts the laptop aside and engages in a natural, uninterrupted conversation. They can maintain eye contact and build rapport, leading to a better patient experience.
- Step 3: Review and Finalize. Shortly after the visit, a structured draft note appears directly in the EHR. The clinician quickly reviews the AI-generated note for accuracy, makes any necessary edits or additions, and signs off. The entire process takes minutes, not hours.
The Proof is in the Data: Real-World Impact and ROI
For healthcare administrators and practice leaders, the decision to invest in new technology must be backed by clear evidence of its value. AI for clinical documentation delivers a powerful, multifaceted return on investment that spans clinical efficiency, financial performance, and quality of care.
Case Study Spotlight: University of Chicago Medicine
A compelling real-world example comes from the University of Chicago Medicine, which rolled out an Abridge-powered ambient AI solution to over 550 clinicians. The results were transformative:
- Clinician Outcomes: In a survey, 90% of participating clinicians reported being able to give their undivided attention to patients, a dramatic increase from 49% before the tool was introduced.
- Patient Outcomes: The impact was also felt by patients. Surveys revealed improvements across multiple areas of the patient experience. Patients provided feedback like, “My doctor is more present in our conversations,” highlighting the restoration of the doctor-patient relationship.
The Financial Equation: Breaking Down the ROI of AI
The financial case for AI in documentation is robust. A 2024 KLAS Research study of 112 healthcare institutions found that organizations implementing these solutions reported an average ROI of 387% within the first year. This return is driven by several key factors:
- Time Savings & Productivity: By saving clinicians 1-2 hours per day, AI allows them to either see more patients or reduces the need for costly overtime. This translates to an estimated annual value of $87,000 to $145,000 per physician from increased patient volume alone.
- Revenue Cycle Enhancement: AI improves the specificity and accuracy of documentation, leading to more appropriate E/M coding and fewer claim denials. This can add $32,000 to $58,000 per provider annually from optimized coding.
- Quality & Risk Reduction: Better documentation supports improved performance in value-based care programs (e.g., more accurate HCC capture for risk adjustment) and reduces medical-legal risk from incomplete records. This can be worth hundreds of thousands of dollars in shared savings and avoided penalties for an organization.
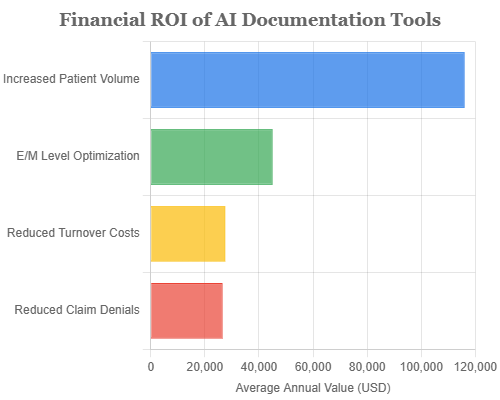
Figure 1: Average annual financial value per physician from implementing AI documentation tools. Data sourced from a comprehensive ROI analysis.
Beyond documentation, AI is driving broader efficiency gains across the clinical tech stack. Discover the role of AI in medical equipment in reshaping patient care delivery.
Navigating the Hurdles: Challenges and Ethical Guardrails
While the benefits are clear, adopting AI for clinical documentation is not without its challenges. A balanced and realistic approach requires acknowledging and planning for these potential hurdles.
Practical and Technical Challenges
- Accuracy is Not Perfection: This is the most critical point. AI-generated notes are drafts and must always be reviewed and signed off by a licensed clinician. A systematic review published in AHIMA noted that “moderate accuracy precludes broad implementation” without rigorous human oversight.
- Integration Complexity: For an AI tool to be effective, it must integrate seamlessly into the existing EHR and clinical workflow. Poor integration can create more friction than it removes, making this a key technical challenge for vendors and health systems.
- Linguistic Diversity: The real world is linguistically complex. Adapting NLP models to accurately understand various accents, dialects, medical jargon, and non-standard phrasing is an ongoing challenge that requires extensive iterative development.
The Ethical and Legal Landscape
- Patient Privacy & Consent: Transparency with patients is non-negotiable. The workflow must begin with clear communication and consent. Furthermore, vendors must provide robust, HIPAA-compliant data security, including encryption and clear data retention policies (e.g., deleting recordings after the note is generated).
- The “Black Box” Problem & Liability: Many advanced AI models operate as a “black box,” where even developers cannot fully explain the reasoning behind a specific output. This raises a critical legal question: if an AI error contributes to patient harm, who is liable? The clinician who signed the note? The software developer? The hospital that implemented the system? This remains a largely unanswered and significant regulatory barrier.
- Maintaining Clinical Skills: Some experts express concern that over-reliance on AI could, over time, erode clinicians’ own documentation and diagnostic reasoning skills. Organizations must consider how to leverage AI as a tool to augment, not replace, clinical judgment.
Frequently Asked Questions (FAQs)
Q1: Will AI for clinical documentation replace human medical scribes and coders?
A: The consensus is that AI will evolve these roles, not eliminate them. AI is best suited for high-volume, repetitive tasks, freeing human experts to focus on more complex cases, quality assurance, auditing the AI’s work, and managing exceptions. AI is expected to enhance their roles, making them more efficient and valuable.
Q2: Is my patient’s data safe?
A: Reputable vendors make this a top priority. They are HIPAA-compliant, use end-to-end encryption, and have strict data handling protocols. For example, some systems delete audio recordings the same day they are used to generate a note. However, healthcare organizations must rigorously vet the security and privacy policies of any vendor before implementation.
Q3: Can patients opt-out of having AI used in their visit?
A: Absolutely. Patient consent is a mandatory and foundational step in any ethical AI documentation workflow. If a patient declines, the visit simply proceeds with traditional documentation methods, with no change to the quality of their care.
Q4: How much time does it really save?
A: Reports vary by specialty and tool, but the savings are consistently significant. Many studies and user testimonials report a reduction of 1-2 hours of documentation time per clinician per day. Some solutions claim to reduce documentation time by up to 76%, effectively eliminating the “pajama time” spent on charts.
Conclusion: The Future of the Clinical Note is Here
Key Takeaways
- The immense burden of clinical documentation is a primary driver of physician burnout, and AI for clinical documentation offers a powerful and proven solution.
- Technologies like ambient AI scribes are fundamentally transforming clinical workflows, allowing clinicians to focus on patients instead of paperwork.
- Successful adoption is a strategic process that requires careful planning, a pilot phase, and a relentless focus on seamless workflow integration.
- While challenges around accuracy, integration, and liability must be managed, the benefits—significant time savings, improved revenue capture, and enhanced patient care—are compelling.
The era of the clinician as a data-entry clerk is coming to an end. The technology to automate documentation is not only here but is maturing rapidly. The future will likely bring even deeper EHR integration, with context-aware AI that can surface predictive insights from clinical notes in real-time. As these tools expand into other areas of healthcare, including nursing and allied health, they promise to unburden clinicians across the care continuum, allowing them to return to the true heart of their profession: caring for patients.
Have you used an AI documentation tool in your practice? What has been your experience? Share your insights or questions in the comments below!