Introduction: A New Dawn in the Fight Against Breast Cancer
Breast cancer is the most commonly diagnosed cancer in women worldwide, with 1 in 8 women in the U.S. expected to develop invasive breast cancer (American Cancer Society, 2024). However, early detection offers hope—when caught at its earliest stage, the 5-year survival rate is 99% (National Breast Cancer Foundation). AI breast cancer detection tools are playing a vital role in making this early diagnosis more accurate and accessible.
While mammography has long been the gold standard for breast cancer screening, it has limitations. High screening volumes can overwhelm radiologists, increasing the risk of human error. One major issue is the “dense tissue dilemma,” affecting over 40% of women—dense tissue and tumors both appear white on mammograms, making cancers harder to spot (DeepLook Medical Study). This can lead to false positives or missed diagnoses. AI breast cancer detection tools are emerging to overcome these challenges, improving accuracy and reducing diagnostic uncertainty.
We are entering a new era in breast cancer care, driven by the transformative power of artificial intelligence. AI breast cancer detection tools are now a clinical reality, offering more than just incremental improvements—they’re revolutionizing diagnosis with greater accuracy, faster workflows, and more personalized care.
This article will explore the intricate technology behind these AI tools, their real-world clinical applications and measurable impact, the critical challenges to their widespread adoption, and the profound, positive change they are bringing to the patient journey.
Table of Contents
The Challenge: Why Early Breast Cancer Detection Is So Difficult
To appreciate the magnitude of AI’s impact, it is essential to first understand the specific hurdles that have long complicated breast cancer screening. These are not minor issues but systemic challenges that affect millions of women and the clinicians dedicated to their care.

A patient undergoing a mammogram on a Hologic Selenia Dimensions system, a standard procedure in breast cancer screening
The Radiologist’s Burden: Radiologists face immense pressure interpreting over 40 million mammograms annually in the U.S. alone (STAT News, 2025). With a global shortage of specialists and rising workloads, diagnostic fatigue becomes a real risk. Early-stage breast cancers often appear as subtle microcalcifications or slight distortions—easy to overlook during repetitive screening. AI breast cancer detection tools help ease this burden by enhancing accuracy and consistency in identifying these early, critical signs.
The Dense Tissue Dilemma: Over 40% of women have dense breast tissue, which significantly reduces the effectiveness of traditional mammograms. Because both dense tissue and cancer appear white on imaging, tumors can be easily hidden—leading to missed diagnoses. This “camouflage effect” is a major reason for false negatives and highlights the urgent need for innovation. AI breast cancer detection tools are addressing this challenge by improving visibility and accuracy in dense breast screenings (Femtech Insider, 2025).
Subtlety and Subjectivity: The interpretation of mammograms involves a degree of subjectivity. What one radiologist might flag as suspicious, another might dismiss as benign. This inter-reader variability is a well-documented phenomenon that can lead to inconsistent patient outcomes (Artificial Intelligence in Breast Cancer Diagnosis and Personalized Treatment Review). The success of a screening often depends on the experience and training of the individual radiologist, introducing a variable that technology can help standardize.
Subtlety and Subjectivity: Mammogram interpretation is inherently subjective—what one radiologist sees as suspicious, another may consider benign. This inter-reader variability can lead to inconsistent diagnoses and patient outcomes (Artificial Intelligence in Breast Cancer Diagnosis and Personalized Treatment Review). AI breast cancer detection tools help reduce this variability by providing standardized, data-driven analysis, supporting more consistent and accurate screenings regardless of the reader’s experience level.
The Consequences of Error: In breast cancer screening, mistakes carry serious weight. False positives can trigger unnecessary imaging and biopsies, leading to “scanxiety” and emotional distress. Even more critical are false negatives—missed cancers that may progress silently to advanced stages with lower survival rates. AI breast cancer detection tools aim to reduce both types of errors, improving diagnostic accuracy and giving patients greater peace of mind.
The AI Revolution: How AI-Powered Imaging Tools Work
Artificial intelligence is not merely a new version of old technology; it is a fundamentally different approach to image analysis. Instead of relying on pre-programmed rules, modern AI systems learn to identify patterns from vast quantities of data, mimicking and, in some cases, exceeding human cognitive abilities for specific tasks.
The Science Behind the Screen: AI Models and Algorithms
At the heart of this revolution are several key technologies that work in concert to analyze medical images with unprecedented sophistication.

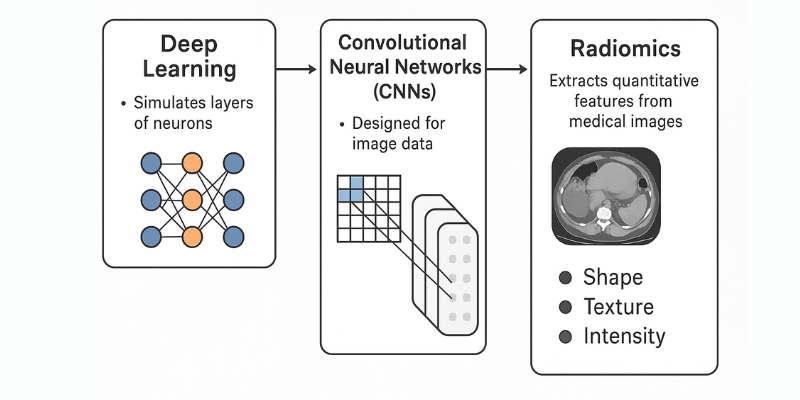
Deep Learning & Convolutional Neural Networks (CNNs): These advanced AI models are the backbone of modern medical imaging. CNNs, inspired by the human brain, learn from vast datasets of labeled mammograms to detect patterns linked to breast cancer. In AI breast cancer detection, CNNs excel at identifying subtle textures and asymmetries that may be invisible to the human eye—making early, accurate diagnosis more achievable (FRONTLINE, 2019).
Radiomics: Radiomics goes beyond simple detection by extracting hundreds of quantitative features—like shape, size, texture, and intensity—from breast images. These features create a “digital signature” of a tumor (Overview of Radiomics in Breast Cancer Diagnosis). In AI breast cancer detection, radiomics allows for non-invasive predictions about tumor aggressiveness, subtype, and treatment response, offering deeper insights without a biopsy.
Differentiating AI Functions: It’s crucial to distinguish between two primary functions of these AI tools:
- Computer-Aided Detection and Diagnosis (CADe/CADx): This is the more established application, where AI acts as a “second reader.” It analyzes a current mammogram to detect and flag suspicious lesions for the radiologist’s review. Modern deep learning-based CADx systems are a significant advancement over older, rule-based CAD systems, which were often plagued by high false-positive rates (Overview of Artificial Intelligence in Breast Cancer Medical Imaging).
- Prognostic and Risk Prediction: This is the new frontier. Instead of just finding existing cancer, these AI models analyze the overall texture and patterns of breast tissue on a completely “normal” screening mammogram to predict a woman’s future risk of developing cancer over a specific period, such as five years. This shifts the paradigm from reactive detection to proactive prevention and personalized screening.
Spotlight on Innovation: Game-Changing AI Tools
The theoretical potential of AI is being realized through a growing number of commercially available and FDA-authorized tools that are now entering clinical practice.
Clairity Breast (Risk Prediction): Clairity Breast is the first AI platform approved by the FDA to predict a woman’s five-year breast cancer risk using only a standard screening mammogram (Breast Cancer Research Foundation, 2025). Unlike traditional models based on self-reported factors like age or family history—which miss 85% of cases—Clairity uses AI to detect subtle, sub-visual patterns in breast tissue. This makes AI breast cancer detection more accurate and equitable, with strong performance across diverse racial and ethnic groups (News-Medical.net, 2025).
DL Precise™ (Enhanced Visualization): DL Precise, developed by DeepLook Medical, is an FDA-cleared AI tool designed to overcome the dense breast tissue challenge. Integrated seamlessly into radiology workflows, it uses shape-recognition AI to enhance lesion visibility and provide single-click segmentation (ITN, 2025). By clarifying tissue boundaries, DL Precise supports more confident decision-making and improves recall rates—making it a valuable advancement in AI breast cancer detection (DeepLook Medical Study).
A Global Ecosystem of Innovation: Clairity and DL Precise are part of a rapidly expanding global field. Other notable tools include:
- Lunit INSIGHT MMG (South Korea): An AI solution for mammography analysis that has been evaluated in numerous studies, including large-scale European trials, showing its ability to detect cancers and reduce radiologist workload (Lunit INSIGHT MMG Study).
- Therapixel’s MammoScreen (France): An AI-powered software that assists radiologists by assigning a unique “suspicion score” to mammograms, helping to prioritize cases and improve reading performance.
- iCAD’s ProFound AI® (USA): One of the leading platforms for both 2D and 3D mammography (tomosynthesis), ProFound AI has been shown to significantly improve cancer detection rates while reducing recall rates and reading time (AI Applications in Breast Imaging Review).
The validation of these tools is not confined to one country. Major prospective studies in nations like Sweden and Germany are providing real-world evidence of AI’s effectiveness, demonstrating that this is a truly global technological movement in healthcare (German Nationwide AI Implementation Study, 2025).
The Clinical Impact: Measurable Improvements in Patient Care
The adoption of AI-powered imaging tools is moving beyond academic research and into clinical practice, delivering tangible, evidence-based benefits that are reshaping the standards of care in breast cancer screening.
Enhancing Diagnostic Accuracy
The primary goal of any screening technology is to find cancer accurately. Here, AI is demonstrating remarkable results. By serving as a tireless, objective second reader, AI helps to both find more cancers and reduce unnecessary alarms.
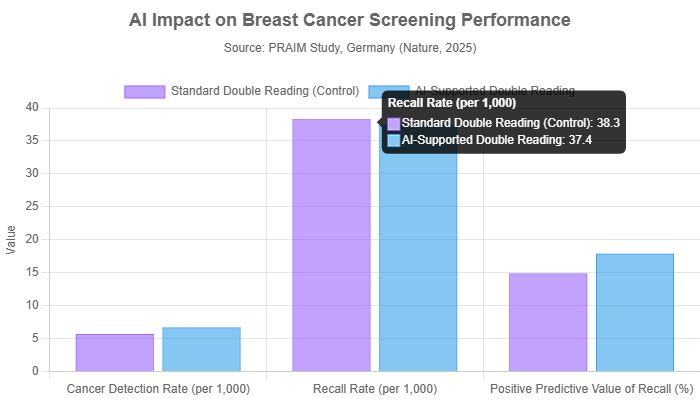
Higher Cancer Detection Rates: A large-scale study from Germany’s national screening program showcased the real-world impact of AI breast cancer detection. Among over 460,000 women, radiologists using AI achieved a cancer detection rate of 6.7 per 1,000—17.6% higher than the 5.7 per 1,000 rate without AI support (PRAIM Study, Nature, 2025). That’s one additional cancer found per 1,000 women screened—a significant improvement in early detection at the population level.
Reducing False Positives and Negatives: In breast cancer screening, accuracy means not just finding more cancers—but avoiding false alarms. AI breast cancer detection excels at both. A Nature study found AI reduced false positives by 5.7% (U.S. dataset) and false negatives by 9.4% (U.K. dataset) compared to human readers (AI Applications in Breast Imaging Review). Similarly, the German PRAIM study showed AI increased cancer detection while slightly lowering recall rates—boosting the positive predictive value of flagged cases.
Tackling Interval Cancers: Interval cancers—diagnosed between regular screenings—are often more aggressive and harder to treat. They represent a critical gap in early detection. AI breast cancer detection is helping close this gap. A UCLA Health study found that AI could identify subtle signs on prior “normal” mammograms, potentially reducing interval cancer rates by up to 30% (UCLA Health, 2025). This predictive ability marks a major shift—catching cancer before it becomes clinically visible.
Streamlining the Radiology Workflow
Beyond accuracy, AI is proving to be a powerful tool for optimizing the entire diagnostic process, making it faster and more efficient.
Workload Reduction and Triage: AI breast cancer detection tools can streamline workflows by pre-screening mammograms and triaging them based on abnormality risk. Studies show AI can automatically clear most normal scans, allowing radiologists to focus on complex cases. This approach may reduce reading workload by over 50% (AI Applications in Breast Imaging Review). In the German PRAIM study, radiologists spent 43% less time reviewing exams pre-identified as normal by AI (Nature, 2025).
Accelerating Diagnosis: Waiting for follow-up after a mammogram can be agonizing. AI breast cancer detection tools offer a solution by triaging high-risk cases for immediate review. A prospective study showed that AI reduced time to additional imaging by 25% and shortened time to biopsy diagnosis by 30%—from 56 days to just 39 (Triaging Mammography with AI Study, 2025). For patients with cancer, this means faster answers and earlier treatment initiation.
The Patient Perspective: A More Empowered and Less Anxious Journey
While the technical and clinical metrics are impressive, the ultimate measure of any medical technology is its impact on patients’ lives. AI-powered imaging is transforming the patient experience by making it less stressful, more personalized, and more hopeful.

AI-powered tools can facilitate clearer and more personalized discussions between doctors and patients
Reducing “Scanxiety”: The emotional toll of waiting for mammogram results—known as “scanxiety”—is real. AI breast cancer detection helps ease this stress by improving accuracy and reducing false-positive recalls. Faster diagnosis through AI triage means less time spent in uncertainty. And knowing a second, highly accurate AI system has reviewed the scan offers patients added peace of mind (CHRISTUS Health).
Personalized Screening Pathways: AI breast cancer detection tools like Clairity Breast are transforming screening from age-based schedules to truly personalized care. These risk-prediction models can identify high-risk women—even without a family history—who may benefit from earlier or more frequent screening, such as annual MRIs (BCRF on Clairity Breast, 2025). Low-risk women might safely extend screening intervals, reducing unnecessary tests and anxiety. This AI-driven approach supports more precise, individualized breast cancer prevention.
Building Trust Through Collaboration: Patient trust in AI breast cancer detection depends on collaboration, not replacement. According to an RSNA survey (2025), only 5% of patients are comfortable with AI interpreting scans alone—but 71% support AI as a second reader alongside a radiologist. This underscores the importance of a hybrid approach, where AI enhances human expertise. Transparency, communication, and maintaining the human connection are key to building patient confidence in AI-supported care.
The Impact of a Life-Saving Catch: Real-world stories highlight the power of AI breast cancer detection. In the U.K., 68-year-old Sheila Tooth had a routine mammogram declared normal by two radiologists. But AI, used in a trial, spotted tiny cancer cells they missed. Caught early, she only needed a minor procedure. “I’m deeply grateful… I just feel so lucky,” she shared (Fox News, 2024). Her case shows how AI can act as a vital safety net—catching what humans may overlook.
Navigating the New Frontier: Challenges and Ethical Considerations
Despite its immense promise, the widespread integration of AI into breast imaging is not without its challenges. Navigating this new frontier requires careful consideration of technical hurdles, ethical questions, and the practicalities of clinical implementation.
Key Challenges in AI Implementation
- Transparency: Overcoming the “black box” nature of AI to ensure clinicians can trust and verify its decisions.
- Data Bias: Ensuring AI models are trained on diverse datasets to prevent health disparities and ensure equitable performance.
- Integration: Seamlessly incorporating AI tools into existing and often complex hospital IT systems (like PACS).
- Regulation & Accountability: Establishing clear regulatory pathways and frameworks for liability and accountability.
The “Black Box” Problem and Explainable AI (XAI): A major barrier to trust in AI breast cancer detection is the lack of transparency in how decisions are made. Explainable AI (XAI) addresses this by using tools like Grad-CAM to create heatmaps on mammograms, showing which areas the AI focused on. This visual feedback helps radiologists understand and verify AI decisions—turning the system from a black box into a trustworthy assistant (Explainable Machine Learning for Breast Cancer Diagnosis).
Data Bias and Health Equity: AI breast cancer detection is only as reliable as the data behind it. If trained mostly on images from one demographic, AI may underperform for others—worsening health disparities (U.S. Preventive Services Task Force). To ensure equity, models must be built and validated on diverse datasets. Clairity, for example, has prioritized inclusive development to ensure accurate results across all racial and ethnic groups (BCRF, 2025).
Regulatory Hurdles and Clinical Integration: Before AI breast cancer detection tools can be used in practice, they must be rigorously validated and FDA-approved—over 20 such tools have been cleared to date (AI Applications in Breast Imaging Review). But approval is just the first step. Successful clinical integration requires seamless compatibility with hospital systems like PACS, demanding close collaboration between AI developers and healthcare providers.
Clinician Trust and Accountability: While radiologists are generally optimistic about AI breast cancer detection, accountability remains a concern—especially in cases of missed diagnoses. Most support AI as a second reader but are cautious about autonomous use, such as triaging without human review (Australian Healthcare Workers’ Views on AI). To build trust, robust clinical trials, clear legal guidelines, and standardized performance metrics are essential.
Frequently Asked Questions (FAQs)
Will AI replace radiologists?
No. The overwhelming consensus among experts and in clinical studies is that AI will augment, not replace, radiologists. The most effective model is a human-AI collaboration, where the technology serves as a powerful “second reader” or a “vigilant assistant.” AI excels at tirelessly sifting through data and detecting subtle patterns, while human radiologists provide critical context, clinical judgment, and direct patient interaction. Patient surveys also strongly support this collaborative model (RSNA, 2025).
Are AI-powered imaging tools safe?
Yes. AI tools intended for clinical use are classified as medical devices and must undergo a rigorous validation and review process by regulatory bodies like the FDA in the United States. This process is designed to ensure the tools are both safe and effective for their intended use. For example, the FDA has granted specific clearances, such as De Novo authorization for novel devices like Clairity Breast, to confirm they meet high standards before they can be marketed to hospitals (FDA AI-Enabled Medical Devices).
How can I get access to AI-assisted mammography?
The availability of AI-powered imaging tools is growing rapidly as more hospitals and imaging centers adopt the technology. However, it is not yet universal. The best approach for patients is to be proactive. You can ask your primary care provider or the staff at your chosen breast imaging center if they utilize AI-assisted technology for either mammogram interpretation (detection) or risk assessment. Organizations like the National Breast Cancer Foundation provide resources to find accredited mammography facilities, which may be early adopters of such technologies (National Breast Cancer Foundation).
Does insurance cover AI-powered breast imaging?
Coverage is currently an evolving landscape. For AI applications that act as a second reader for a standard screening mammogram, the cost is often bundled into the existing reimbursement for the mammogram itself. However, for newer, distinct applications like AI-based risk prediction, coverage is not yet standard. Companies like Clairity are actively working with insurance providers and Medicare to establish reimbursement pathways, but initially, some of these advanced services may be offered on a self-pay basis (BCRF, 2025). Patient and provider advocacy will be key to expanding access.
Conclusion: Empowering the Future of Breast Cancer Care with AI
TThe integration of AI-powered imaging tools into breast cancer care represents a transformative shift—from reactive diagnosis to proactive, personalized, and predictive medicine. These technologies aren’t just improving statistics—they’re reshaping patient experiences and outcomes.
With higher diagnostic accuracy, faster workflows, and reduced patient anxiety, AI breast cancer detection is elevating standard mammograms into precision tools that can anticipate risk and detect cancer earlier than ever before.
While challenges like data bias, explainability, and clinical integration persist, they can be addressed through collaboration between developers, clinicians, regulators, and patients. The goal isn’t to replace radiologists but to empower them—combining human expertise with machine intelligence to save lives.
Together, we stand on the brink of a future where breast cancer is caught earlier, treated faster, and feared less.
💡 Want to learn more?
Check out our related article:
👉 Early Signs of Breast Cancer: How to Spot the First Symptoms
Stay informed about the latest advancements in medical technology. Follow MedTech Insighter for more deep dives into how innovations like AI are shaping the future of healthcare. Share this article to spread awareness about the power of AI in the fight against breast cancer.