Introduction
As a Senior Biomedical Engineer with over 19 years of experience, I’ve spent my career at the intersection of technology and human health. I’ve seen firsthand how intricate the human body is, particularly the immune system—our personal, highly-intelligent defense force. But what happens when this defense system turns against the very body it’s designed to protect? This is the reality for millions of people worldwide living with autoimmune diseases.
From fatigue and joint pain that seem to have no clear origin to more specific conditions like lupus, rheumatoid arthritis, or Hashimoto’s thyroiditis, autoimmune diseases are complex, often misunderstood, and can be incredibly challenging to diagnose and manage. The journey for patients is frequently long and frustrating, marked by a search for answers and relief.
This article aims to be a comprehensive, evidence-based resource for anyone touched by autoimmunity—whether you’re a patient seeking answers, a caregiver supporting a loved one, a healthcare student, or simply someone passionate about wellness. We will demystify autoimmune diseases by exploring:
- What they are and their common symptoms.
- The underlying causes, including genetics, environment, and the crucial role of gut health.
- Powerful, natural strategies centered on diet and lifestyle that can help manage symptoms and rebalance the immune system.
- Real-world examples and answers to your most pressing questions.
Our goal is to empower you with knowledge, bridging the gap between medical science and practical, everyday wellness. Let’s dive in.
Table of Contents
What Are Autoimmune Diseases?
At its core, an autoimmune disease is a condition where your body’s immune system mistakenly attacks its own healthy cells, tissues, and organs. Normally, the immune system is a vigilant guardian, identifying and destroying foreign invaders like bacteria, viruses, and toxins. In autoimmunity, this system loses its ability to distinguish between “self” and “non-self,” leading it to launch an attack on its own body.
Autoimmune diseases can strike almost any part of the body—from the skin and joints to the thyroid and nervous system. According to the National Institutes of Health (NIH), over 80 autoimmune diseases exist. Some target specific organs, like Type 1 diabetes affecting the pancreas, while others, such as lupus, attack multiple systems at once.
Most of these conditions are characterized by chronic inflammation, which is the body’s natural response to injury or infection. When this response is constant, it leads to the common signs of redness, heat, pain, and swelling that many patients experience.
Common Symptoms: The Body’s Vague Alarms
One of the biggest challenges in diagnosing autoimmune diseases is that early symptoms are often non-specific and can mimic other conditions. They can also come and go, with periods of intense symptoms (known as flare-ups) followed by periods of remission where symptoms lessen or disappear. According to Johns Hopkins Medicine, some of the most common early symptoms include:
- Fatigue: A profound, persistent exhaustion that isn’t relieved by rest.
- Joint pain and swelling: Often one of the first signs, particularly in conditions like rheumatoid arthritis.
- Skin problems: Rashes, sensitivity to sun, or patches of discolored skin.
- Abdominal pain or digestive issues: Linked to conditions like Crohn’s disease or celiac disease.
- Recurring low-grade fever: The body’s inflammatory response running in the background.
- Swollen glands: A sign that the immune system is in overdrive.
- Trouble concentrating or “brain fog.”
Because these symptoms are so general, the journey to a diagnosis can be long and frustrating for many patients.
Who is at Risk?
While the exact causes are still being researched, several factors are known to increase the risk of developing autoimmune diseases:
- Gender: Women are significantly more likely to develop autoimmune diseases than men. MedlinePlus notes that this disparity is a key area of research.
- Genetics: These conditions often run in families. Having a relative with an autoimmune disease increases your risk, suggesting a genetic predisposition.
- Existing Autoimmune Disease: If you have one autoimmune condition, you are at a higher risk of developing another. For example, there is a well-documented link between Hashimoto’s thyroiditis and other conditions like lupus or rheumatoid arthritis .
- Environmental Factors: Exposure to infections, toxins, and even certain dietary components can act as triggers in genetically susceptible individuals.
The Scientific Deep Dive: How Does the Immune System Go Wrong?
To understand how to manage autoimmunity, we first need to explore the mechanisms behind this immune system malfunction. The loss of self-tolerance—the immune system’s ability to ignore its own tissues—is a central event. Researchers believe several processes contribute to this breakdown.
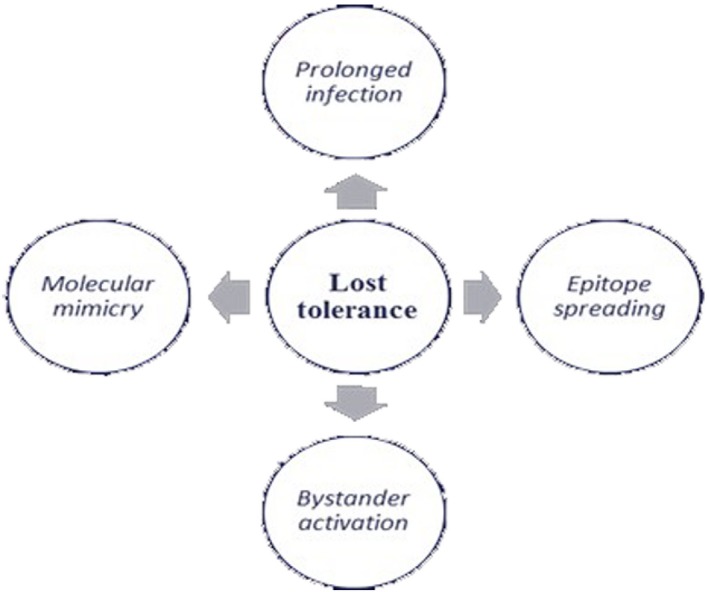
- Molecular Mimicry: A foreign invader (like a virus or bacterium) may have proteins that look very similar to proteins found in the human body. The immune system mounts an attack against the invader, but in the process, it also learns to attack the similar-looking “self” proteins.
- Bystander Activation: During a major infection, the immune system releases a flood of inflammatory signals to activate as many immune cells as possible. This massive, non-specific activation can sometimes awaken dormant self-reactive immune cells, which then begin to attack the body’s own tissues.
- Epitope Spreading: When an initial autoimmune attack damages a specific tissue, it releases new, previously hidden self-proteins. The immune system may then recognize these newly exposed proteins as foreign and launch a secondary attack, broadening the scope of the autoimmune response.
- Intestinal Permeability (“Leaky Gut”): This is a critical factor that has gained significant attention. The lining of our gut is supposed to be a tight barrier, controlling what gets absorbed into the bloodstream. When this barrier becomes compromised (or “leaky”), undigested food particles, toxins, and microbes can pass into the bloodstream, triggering a systemic immune and inflammatory response. Many researchers believe this is a key prerequisite for the development of autoimmunity .
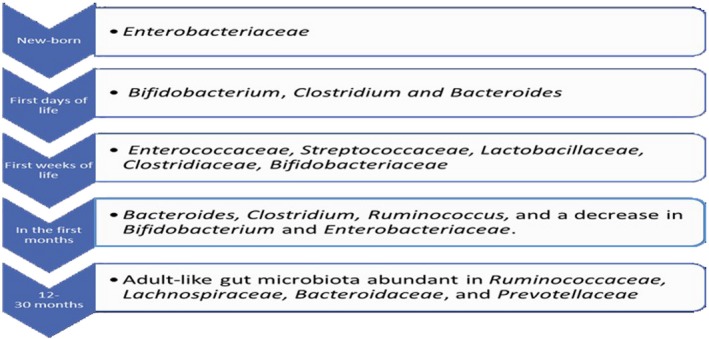
The Gut Microbiome: The Command Center for Immunity
The connection between gut health and autoimmune diseases cannot be overstated. Our gut is home to trillions of microorganisms—bacteria, viruses, and fungi—collectively known as the gut microbiome. This ecosystem plays a fundamental role in educating and regulating our immune system. A healthy, diverse microbiome promotes immune tolerance.
However, factors like a poor diet, stress, antibiotics, and infections can disrupt this delicate balance, a condition called dysbiosis. Dysbiosis is consistently linked to autoimmune conditions. For example, studies have shown that patients with rheumatoid arthritis often have an overgrowth of certain bacteria like Prevotella copri, while patients with lupus may have a lower ratio of Firmicutes to Bacteroidetes bacteria . This imbalance can promote inflammation and contribute to the leaky gut phenomenon, creating a vicious cycle that fuels autoimmunity.
Natural Management: Rebalancing Your Immune System Through Lifestyle
While there is no cure for most autoimmune diseases, a growing body of evidence shows that diet and lifestyle interventions can significantly reduce inflammation, manage symptoms, and improve quality of life. These approaches focus on healing the gut, calming the immune system, and providing the body with the nutrients it needs to thrive. It’s crucial to remember that these strategies should complement, not replace, medical treatment. Always consult your healthcare provider before making significant changes.
1. The Power of an Anti-Inflammatory Diet
The cornerstone of naturally managing autoimmunity is adopting an anti-inflammatory diet. The goal is to remove foods that trigger inflammation and replace them with nutrient-dense, whole foods that heal the body. The Arthritis Foundation and Harvard Health both recommend diets rich in fruits, vegetables, healthy fats, and lean proteins.

Foods to Embrace:
- Leafy Green Vegetables: Spinach, kale, and collards are packed with antioxidants and vitamins.
- Colorful Fruits & Vegetables: Berries, carrots, squash, and broccoli contain polyphenols and carotenoids, which are powerful anti-inflammatory compounds .
- Healthy Fats: Omega-3 fatty acids found in fatty fish (salmon, mackerel), flaxseeds, and walnuts are known to reduce inflammation. Olive oil is another excellent source of healthy fat.
- Fiber-Rich Foods: Whole grains, legumes, and vegetables feed beneficial gut bacteria and help lower C-reactive protein (CRP), a marker of inflammation in the blood.
- Lean Proteins: Poultry, fish, and plant-based proteins like lentils and beans.
- Herbs and Spices: Turmeric, ginger, cinnamon, and garlic all have potent anti-inflammatory properties.
Foods to Avoid or Limit:
- Processed and Refined Foods: These often contain unhealthy fats, sugar, and additives that promote inflammation.
- Added Sugars and Refined Carbohydrates: White bread, pastries, sodas, and sugary snacks can spike blood sugar and drive inflammatory pathways.
- Certain Fats: Trans fats (found in fried foods and many processed snacks) and an excess of omega-6 fatty acids (found in vegetable oils like corn, soy, and sunflower oil) can be pro-inflammatory.
- Processed Meats: Sausages, bacon, and deli meats are often high in sodium and preservatives that can trigger inflammation.
- Dairy and Gluten (for some): These are common sensitivities for people with autoimmune conditions and can contribute to gut inflammation. An elimination diet can help determine if they are a problem for you.
2. The Autoimmune Protocol (AIP) Diet: A Deeper Dive
For those who don’t find sufficient relief with a general anti-inflammatory diet, the Autoimmune Protocol (AIP) diet can be a powerful therapeutic tool. As described by Healthline, the AIP is a stricter, temporary elimination diet designed to heal the gut lining and identify specific food triggers.
The AIP diet works in two main phases:
Phase 1: The Elimination Phase
This phase involves removing all foods that could potentially irritate the gut and stimulate the immune system. This is typically followed for 30-90 days, or until symptoms have noticeably improved. Foods to eliminate include:
- All grains (wheat, rice, oats, corn)
- All legumes (beans, lentils, peanuts, soy)
- All dairy products
- Eggs
- Nuts and seeds
- Nightshade vegetables (tomatoes, potatoes, peppers, eggplant)
- Processed sugars, oils, and food additives
- Alcohol and coffee
The focus is on consuming nutrient-dense whole foods like quality meats and fish, a wide variety of vegetables (excluding nightshades), fruits (in moderation), healthy fats like olive and avocado oil, and fermented foods.
Phase 2: The Reintroduction Phase
Once symptoms have improved, foods are slowly and systematically reintroduced one at a time. This allows you to identify which specific foods trigger a reaction. A food is typically reintroduced over several days while you monitor for any return of symptoms. This personalized approach helps you build a long-term diet that is right for your body.
The goal of the AIP diet is not to be restrictive forever, but to gather data. It’s a short-term strategy to identify your personal triggers and create a sustainable, nourishing diet for long-term health.
3. Key Supplements and Herbal Support
While diet is foundational, certain supplements and herbs can provide additional support. However, it’s vital to approach supplements with caution.
Beneficial Supplements (Under Medical Guidance):
- Curcumin (from Turmeric): A potent anti-inflammatory. Studies, particularly in lupus and RA, have shown that curcumin can suppress inflammatory pathways like NF-κB and may help reduce symptoms like proteinuria in lupus nephritis .
- Omega-3 Fish Oil: Helps to balance the omega-6 to omega-3 ratio, reducing overall inflammation.
- Vitamin D: Many people with autoimmune conditions are deficient in Vitamin D, which is a crucial immune modulator.
- Probiotics: Specific strains of Lactobacillus and Bifidobacterium can help restore gut flora balance, strengthen the gut barrier, and modulate the immune response. A 2024 meta-analysis in BMC Medicine found that gut microbiota-based therapies may improve several autoimmune diseases.
- Polyphenols: These compounds found in plants (like resveratrol from grapes and EGCG from green tea) have antioxidant and immunomodulatory effects .
A Word of Caution on “Immune-Boosting” Supplements
It’s tempting to reach for supplements marketed as “immune boosters.” However, for someone with an autoimmune disease, stimulating an already overactive immune system can be counterproductive and may even trigger a flare. Herbs like Echinacea, Spirulina, Chlorella, and Alfalfa have immunostimulatory properties and should generally be avoided by those with autoimmune conditions . Always discuss any new supplement with your doctor.
4. Lifestyle: The Non-Negotiable Foundations
Managing autoimmune diseases goes beyond diet. Stress, poor sleep, and a sedentary lifestyle can all fuel inflammation.
- Stress Management: Chronic stress floods the body with cortisol, an inflammatory hormone. Practices like mindfulness, meditation, yoga, deep breathing, and spending time in nature are essential for calming the nervous system.
- Prioritizing Sleep: Sleep is when the body repairs itself. Aim for 7-9 hours of quality sleep per night. Lack of sleep disrupts immune function and increases inflammatory markers.
- Gentle Movement: While intense exercise can be stressful during a flare, gentle movement like walking, swimming, or tai chi can reduce joint stiffness, improve mood, and lower inflammation.
Living with an autoimmune disease is a journey, much like recovering from cancer — both demand emotional strength, patience, and lifestyle adjustments. If you want to learn practical ways to rebuild confidence and mental health after a major illness, explore our post on Life After Cancer: How to Manage Side Effects and Rebuild Mental Health
Pros & Cons of Natural Approaches
Adopting a natural approach to managing autoimmune diseases offers many benefits, but it’s important to have a balanced perspective.
Pros
- Empowering: Gives you a sense of control over your health.
- Holistic: Addresses the root causes of inflammation rather than just masking symptoms.
- Fewer Side Effects: Diet and lifestyle changes are generally safe and have positive side effects (e.g., weight loss, more energy).
- Addresses Comorbidities: Can help manage other conditions often associated with autoimmunity, like metabolic syndrome and hypertension.
- Cost-Effective: Can be less expensive than long-term reliance on certain medications .
Cons
- Not a Cure: These approaches manage symptoms but do not cure the underlying disease.
- Requires Commitment: Significant lifestyle changes require dedication, time, and effort.
- Not a Replacement for Medicine: For many, especially those with severe disease, medication is essential to prevent organ damage.
- Can Be Socially Isolating: Restrictive diets can make social gatherings and dining out challenging.
- Potential for Nutrient Deficiencies: Highly restrictive diets like AIP should be done with guidance to avoid nutritional gaps.
The Future: Emerging Therapies
While lifestyle interventions are powerful, the field of biomedical engineering and immunology is rapidly advancing. Exciting new treatments are on the horizon that offer more targeted ways to correct the immune system. These therapies aim to re-establish tolerance with greater precision.
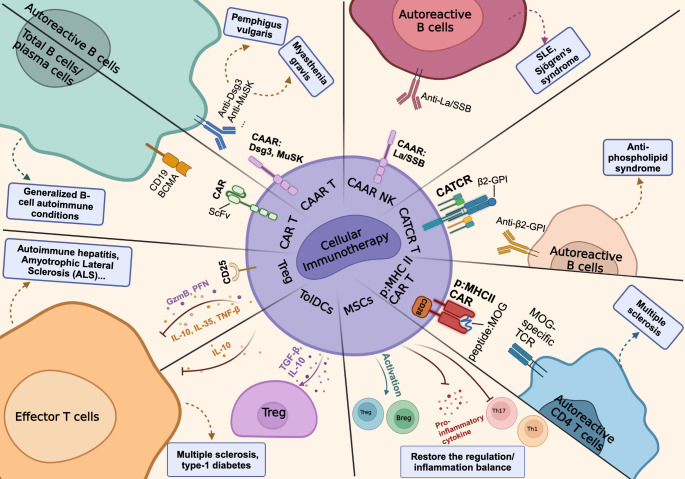
One of the most promising areas is cellular immunotherapy. Originally developed for cancer, therapies like CAR-T (Chimeric Antigen Receptor T-cell) therapy are now being adapted for autoimmune diseases. In this approach, a patient’s own T-cells are engineered in a lab to recognize and destroy the B-cells that produce harmful autoantibodies. Early clinical trials for severe lupus have shown remarkable success, leading to drug-free remission in some patients . These targeted therapies represent a paradigm shift from broad immune suppression to precise immune correction.
Frequently Asked Questions (FAQs)
1. Can autoimmune diseases be cured?
Currently, there is no known cure for most autoimmune diseases. The goal of treatment—both medical and natural—is to manage symptoms, reduce inflammation, and induce remission, which is a period where the disease is inactive. Some people can achieve long-term remission and live symptom-free lives.
2. Are natural remedies a replacement for my medication?
No. Natural and lifestyle approaches should be seen as a powerful complement to your medical treatment, not a replacement. Never stop or change your medication without consulting your healthcare provider. The goal is an integrative approach that combines the best of both worlds.
3. How long does it take for diet changes to work?
This varies greatly from person to person. Some people notice improvements in a few weeks, while for others it may take several months. Consistency is key. The goal is to reduce inflammation and heal the gut, which is a gradual process.
4. What is the life expectancy for someone with an autoimmune disease?
This depends heavily on the specific disease and its severity. Many people with autoimmune conditions live full, normal lifespans. However, some diseases like multiple sclerosis or severe lupus can have life-threatening complications. According to the Cleveland Clinic, managing the disease effectively with your healthcare team is the best way to ensure a positive long-term outlook.
AI and Early Diagnostic Technologies in Autoimmune Disorders
Artificial Intelligence is rapidly transforming the way autoimmune diseases are detected. By analyzing large datasets from medical records, genomics, and imaging, AI algorithms can identify subtle patterns long before symptoms appear. Predictive models are now helping clinicians detect autoimmune markers earlier, personalize treatment plans, and monitor disease progression with greater accuracy. This integration of AI into immunology could soon make early diagnosis faster, cheaper, and more reliable — reducing complications and improving patient quality of life.
Conclusion: Taking Control of Your Health Journey
Living with an autoimmune diseases is a journey, but it doesn’t have to be one of passive suffering. While the diagnosis can feel overwhelming, understanding the interplay between your immune system, your gut, and your lifestyle is the first step toward reclaiming your health.
By adopting an anti-inflammatory, nutrient-dense diet, identifying personal food triggers, managing stress, and prioritizing sleep and movement, you can create an internal environment that promotes healing and balance. These natural strategies, used in partnership with your medical team, can profoundly impact your quality of life, reduce symptoms, and empower you to thrive.
Remember, you are the expert on your own body. Listen to its signals, be patient with the process, and celebrate every step forward.
Medical Disclaimer
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before making medical decisions.