Introduction: Your Liver’s Second Chance is Within Reach
Did you know that about 1 in 3 adults worldwide has a hidden condition that can seriously harm their long-term health? It’s called fatty liver disease, and it’s rising fast—especially with growing rates of obesity, diabetes, and poor diets.
Doctors now often refer to it as MASLD (Metabolic Dysfunction-Associated Steatotic Liver Disease), but the root issue stays the same: too much fat builds up in your liver—not from alcohol, but from lifestyle and diet. Left unchecked, it can lead to inflammation, scarring, and even liver failure (PMC, 2019)
The good news? You can reverse it—naturally.
While there’s no specific medication yet, simple lifestyle changes are proven to heal your liver. In this guide, you’ll learn:
- What fatty liver is and why it happens
- How the right diet and exercise can reverse it
- What foods to eat (and avoid)
- Real-life success stories
- And a clear, step-by-step plan to get started today
Table of Contents
What is Fatty Liver Disease? A Quick Look at the “Silent” Epidemic
Before we talk about reversing fatty liver, let’s understand why it’s a big deal. Your liver is a powerhouse—handling over 300 critical functions like filtering toxins, storing nutrients, and keeping your metabolism in check. When your liver is unhealthy, it doesn’t just affect digestion—it can throw your entire body off balance.
Defining NAFLD/MASLD: More Than Just a Name Change
Fatty liver disease happens when too much fat builds up in your liver cells. A small amount of fat is normal—but when it makes up more than 5–10% of your liver’s weight, it’s called steatosis, or fatty liver (American Liver Foundation, 2025).
This condition isn’t all-or-nothing—it exists on a spectrum, ranging from mild to serious, depending on how much damage and inflammation is present.
- Simple Fatty Liver (NAFL or MASL): This is the initial stage where there is excess fat in the liver but little to no inflammation or liver cell damage. Many people have this condition without knowing it.
- Nonalcoholic Steatohepatitis (NASH or MASH): This is a more advanced and dangerous form. In addition to excess fat, there is inflammation and liver cell damage. It is estimated that about 20% of people with simple fatty liver will progress to NASH. This inflammation and damage can lead to fibrosis (scarring), cirrhosis, and even liver cancer.
What makes this disease especially dangerous is its “silent” nature—most people with NAFLD have no symptoms, especially in the early stages. When signs do appear, they’re often vague and easy to ignore, like fatigue or a dull ache in the upper right side of the abdomen, which can delay diagnosis and treatment (NIDDK).
Why It Matters: The Key Risk Factors
NAFLD isn’t random—it’s closely tied to poor metabolic health. Key risk factors include obesity, insulin resistance, type 2 diabetes, and high blood fats. Identifying these is the first step to prevention and recovery.

- Overweight or Obesity: This is the most common risk factor. Fat centered in the waist (abdominal obesity) is particularly strongly linked to NAFLD.
- Insulin Resistance & Type 2 Diabetes: Insulin resistance, where your cells don’t respond properly to the hormone insulin, is a central driver of the disease. It leads to increased fat storage in the liver.
- Metabolic syndrome: This is a group of conditions—high blood pressure, high blood sugar, belly fat, and abnormal cholesterol or triglycerides—that, when combined, greatly increase your risk of developing fatty liver.
- Abnormal Blood Fat Levels: High levels of triglycerides, a type of fat in your blood, are a major contributor (Mayo Clinic, 2024).
- High Intake of Added Sugars: Diets high in sugar, particularly high-fructose corn syrup found in many processed foods and drinks, are strongly associated with the development of fatty liver.
- Lean NAFLD: It’s important to note that you don’t have to be overweight to develop NAFLD. “Lean NAFLD” can affect individuals with a normal Body Mass Index (BMI), often due to factors like high fructose intake, genetics, or even weight gain within a “normal” range.
The Core Strategy: Reversing Fatty Liver Through Your Diet
Decades of research point to one clear truth: diet is the most powerful tool for managing and reversing fatty liver disease. Since it’s closely linked to metabolic health, what you eat directly affects liver fat and inflammation.
The Foundation: Weight Management is Key
For people with NAFLD who are overweight or obese, the main treatment goal is gradual, sustainable weight loss. This doesn’t mean crash diets—it means creating a steady, manageable calorie deficit your body can maintain, which has been consistently shown to improve liver health.
Clinical guidelines show that losing just 3–5% of your body weight can start reducing liver fat, while a 7–10% loss is often needed to lower inflammation and improve liver function. For those with liver scarring (fibrosis), even greater weight loss—over 10%—may be required to see real improvement.
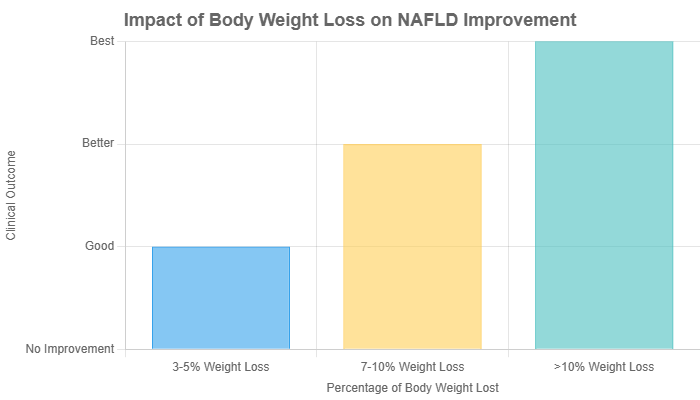
Data sourced from clinical guidelines shows a dose-dependent relationship between weight loss and liver health improvement (AASLD, EASL-EASD-EASO).
The Gold Standard: Adopting the Mediterranean Diet
The Mediterranean diet is the top eating plan recommended for reversing fatty liver. It’s not a restrictive diet, but a sustainable lifestyle built around whole, nutrient-rich foods and minimal processed ingredients—making it highly effective for reducing liver fat.
The Mediterranean diet is characterized by:
- An emphasis on plant-based foods: fruits, vegetables, whole grains, legumes, and nuts.
- Replacing butter and other saturated fats with healthy fats, primarily olive oil.
- Using herbs and spices instead of salt to flavor foods.
- Eating fish and poultry at least twice a week.
- Limiting red meat to only a few times per month.
- Limiting sweets and sugary drinks to special occasions.
This approach works because it naturally lowers inflammation, improves insulin sensitivity, and provides a wealth of antioxidants, all of which directly benefit the liver.
Foods to Embrace: Your Liver-Friendly Shopping List
Building a diet to reverse fatty liver is about focusing on what you *can* eat, not just what you can’t. Here are the food groups that should become staples in your kitchen, based on strong scientific evidence.

Healthy Fats
Swapping unhealthy fats for healthy ones is crucial. Focus on unsaturated fats, which help reduce inflammation. Good sources include:
- Olive Oil: Some experts recommend up to four tablespoons per day. It’s a cornerstone of the Mediterranean diet (UChicago Medicine, 2021).
- Fatty Fish: Salmon, sardines, and tuna are rich in omega-3 fatty acids, which can help lower liver fat and reduce inflammation.
- Nuts and Seeds: Walnuts and sunflower seeds (a great source of the antioxidant Vitamin E) are excellent choices.
- Avocados: Rich in healthy fats and fiber.
Lean Proteins
Protein helps with satiety and muscle maintenance. Choose lean sources:
- Fish and Poultry: As mentioned, fatty fish is ideal. Skinless chicken or turkey are also good options.
- Beans and Legumes: Studies have shown that diets rich in legumes can help lower the likelihood of NAFLD. They are high in fiber and plant-based protein.
- Tofu: A low-fat, high-protein option that can help lower triglyceride levels.
Fiber-Rich Foods
Fiber helps control blood sugar and promotes a feeling of fullness. Aim for:
- Oatmeal and Whole Grains: Choose brown rice, quinoa, and whole-wheat bread over their refined white counterparts.
- Leafy Greens: Compounds in spinach, especially when eaten raw, may help fight fatty liver disease. Kale and other greens are also beneficial.
- Other Vegetables: Broccoli, carrots, and garlic are packed with beneficial compounds.
The Surprise Liver Protectors
- Coffee: This might be the most pleasant surprise. Multiple studies suggest that drinking coffee can help protect your liver. Some dietitians recommend up to three cups of black coffee per day for patients with NAFLD.
- Turmeric: The active compound, curcumin, has antioxidant and anti-inflammatory properties that may reduce markers of liver damage.
Foods to Limit or Avoid: The “Red List” for Your Liver
Just as important as what you add to your diet is what you remove or drastically reduce. These are the primary culprits that contribute to fat accumulation and inflammation in the liver.

- Added Sugars: This is arguably the worst offender. Be vigilant about avoiding sugary drinks like sodas and fruit juices, as well as candy, cookies, and pastries. Added sugars, especially fructose, are a prime culprit in driving liver fat buildup.
- Refined Carbohydrates: White bread, white rice, and white pasta lack fiber and can spike your blood sugar, contributing to fat storage.
- Saturated and Trans Fats: These unhealthy fats are abundant in fried foods, fast food burgers, and many processed snacks. They are a poor choice for liver health.
- Processed and Red Meats: Beef, pork, bacon, and sausages are high in saturated fat and should be limited.
- Alcohol: While the disease is “non-alcoholic,” alcohol still puts extra stress on the liver. Most guidelines recommend that patients with NAFLD abstain from alcohol to avoid further damage.
The Power of Movement: Exercise as Medicine for Your Liver
Diet is only part of the solution—exercise is just as essential. Physical activity works like medicine, tackling the metabolic issues behind fatty liver and offering benefits that go well beyond just burning calories.
Why Exercise is Non-Negotiable
Exercise offers powerful benefits for fatty liver—even without major weight loss. Research shows that simply being more active can reduce liver fat, regardless of body weight, making physical activity a key part of managing and improving the condition.
How does it work? Exercise tackles the root causes by:
- Improving insulin sensitivity: It is one of the key benefits of regular exercise—it helps your muscles use glucose more efficiently, easing pressure on the pancreas and lowering insulin levels, which reduces the signals that trigger fat storage in the liver.
- Increasing Fat Oxidation: Exercise encourages the liver to burn its stored fat for energy.
- Reducing Inflammation: Physical activity has a natural anti-inflammatory effect, which can help calm the inflammation associated with the more severe form, NASH.
Crafting Your Weekly Exercise Plan
Clinical guidelines recommend a combination of two types of exercise for maximum benefit. The key is consistency. The best exercise plan is one you enjoy and can stick with long-term.
Aerobic (Cardio) Exercise
This type of exercise raises your heart rate and improves your body’s use of oxygen. It is particularly effective for heart health and burning calories.
- Goal: Aim for 150-300 minutes of moderate-intensity activity per week (Exercise and Sports Science Australia).
- What is “Moderate Intensity”? You should be able to talk, but not sing, during the activity. Think of it as a brisk walk.
- Examples: Brisk walking, cycling (outdoors or stationary), swimming, water aerobics, dancing, or jogging.

Resistance (Strength) Training
This type of exercise involves working your muscles against a force. It is vital for building muscle mass, which improves your metabolism and insulin sensitivity.
- Goal: At least two days per week, working all major muscle groups (legs, hips, back, abdomen, chest, shoulders, and arms).
- What is the right intensity? You should perform exercises to the point where you feel you need a short rest before doing another repetition.
- Examples: Lifting weights, using resistance bands, bodyweight exercises (like squats, push-ups, and lunges), yoga, and Pilates (British Liver Trust).

Important Note: Before starting any new exercise program, it is crucial to consult with your doctor, especially if you have other health conditions. They can help you create a plan that is safe and effective for you.
Real Stories of Reversal: Inspiration for Your Journey
The science and recommendations are clear, but sometimes the most powerful motivation comes from seeing that real people have successfully walked this path. These stories, based on accounts shared by medical centers and foundations, show that taking control of your lifestyle can lead to life-changing results.

Case Study 1: The Power of Diet and Determination
Kerry, a 38-year-old woman, was diagnosed with NAFLD that had progressed to cirrhosis. Faced with a serious prognosis, she decided to take decisive action. With support from a specialized clinic, she completely revamped her diet and began exercising regularly. As described by UChicago Medicine, Kerry “took the bull by the horns.” Over the course of 18 months, she lost 100 pounds, successfully halted the progression of her cirrhosis, and reversed her fatty liver disease. Her doctor noted that she extended her own life through her dedication, serving as an inspiration and a perfect example of why early action is transformational.
Case Study 2: A Second Chance After a Wake-Up Call
Chris received a serious liver disease diagnosis that served as a profound wake-up call. Frustrated by his symptoms and prognosis, he committed to a complete lifestyle overhaul. He stopped smoking, remained teetotal, adopted a healthier diet, and started exercising. As he shared with the British Liver Trust, the change wasn’t instant, but it was steady. Over two and a half years, his liver gradually repaired itself. It returned to a normal size, and much of the scarring and fat disappeared. He reflects that without these changes, he might have needed a transplant or worse. His story is a powerful testament to the liver’s remarkable capacity for recovery when given the right conditions.
Debunking Common Myths About Fatty Liver
Misinformation can be a significant barrier to progress. Let’s clear up some of the most common myths surrounding fatty liver disease with facts grounded in scientific evidence.
Myth #1: “Liver cleanses or detox supplements will fix my fatty liver.”
“A liver cleanse will help get my liver healthy.”
Fact: This is a dangerous misconception. Your liver is your body’s master detoxification system; it doesn’t need “cleansing” from external products. Johns Hopkins Medicine experts state that liver cleanses have not been proven to treat existing liver damage. In fact, many of these unregulated supplements can be harmful and cause further injury to the liver. The only true “detox” for a fatty liver is a healthy diet, regular exercise, and avoiding substances that stress it, like alcohol and unnecessary medications.
Myth #2: “Only overweight people get fatty liver disease.”
“I have a normal weight, so I can’t have fatty liver.”
Fact: While being overweight or obese is the biggest risk factor, it is not the only one. A significant number of people with a normal BMI develop what is known as “lean NAFLD.” The Liver Foundation notes that poor dietary habits, genetic predisposition, and metabolic disorders can cause fatty liver even in lean individuals. This highlights that diet quality, not just body weight, is a critical factor.
Myth #3: “Fatty liver disease is not reversible.”
“Once you have it, the damage is done forever.”
Fact: This is perhaps the most important myth to bust. In its earlier stages, before significant and advanced scarring (cirrhosis) has developed, fatty liver disease is highly reversible. Countless studies and patient stories confirm that dedicated lifestyle changes can reduce liver fat, calm inflammation, and restore the liver to a healthy state. The key is taking action before the damage becomes permanent.
Myth #4: “To fix a ‘fatty’ liver, I must eat a no-fat diet.”
“All fat is bad for my liver.”
Fact: The *type* of fat you eat is far more important than the total amount. A key principle of the recommended Mediterranean diet is replacing unhealthy fats with healthy ones. The goal is not to eliminate fat, but to choose the right kinds. It is crucial to avoid unhealthy saturated and trans fats found in fried and processed foods. However, incorporating healthy monounsaturated and polyunsaturated fats from sources like olive oil, avocados, nuts, and fatty fish is a cornerstone of the solution, as these fats have anti-inflammatory properties.
Conclusion: Your Action Plan for a Healthier Liver
Reversing fatty liver isn’t about quick fixes—it’s about taking control through small, consistent lifestyle changes. The science is clear: with a whole-foods diet like the Mediterranean plan and regular physical activity, you can tackle the root causes of the disease and give your liver the tools it needs to heal and thrive naturally.
Your 4-Step Action Plan for a Healthier Liver:
- Consult Your Doctor: The first step is always to get a proper diagnosis and professional guidance. Work with your healthcare team to understand your specific situation and rule out other liver conditions.
- Adopt a Mediterranean Diet: Ditch the processed foods, sugary drinks, and excess red meat. Fill your plate with vegetables, lean proteins, whole grains, and healthy fats from olive oil, nuts, and fish.
- Get Moving: Find activities you enjoy and make them a non-negotiable part of your week. Aim for a mix of aerobic exercise (like brisk walking) and strength training.
- Be Patient & Consistent: Reversing liver damage takes time and dedication. There will be challenges, but consistency is your greatest ally. Celebrate small victories and focus on building habits that will last a lifetime.
Your diagnosis can be a wake-up call—but it can also be the beginning of a healthier, more empowered life. If you’re managing a chronic condition, you might also find value in our guide on life after cancer, including how to handle side effects and emotional health.
Medical Disclaimer
This article is for educational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider before making medical decisions.
